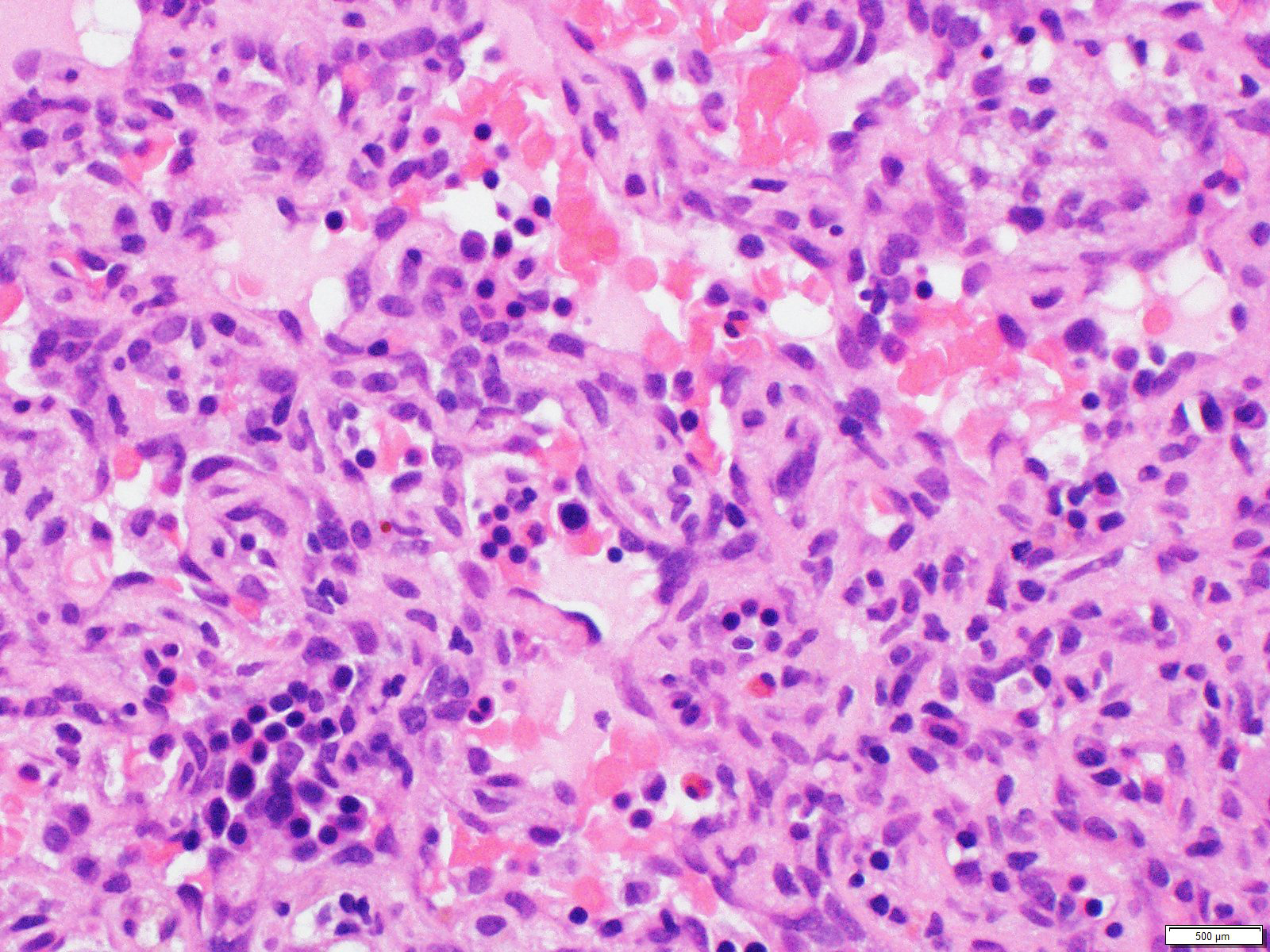
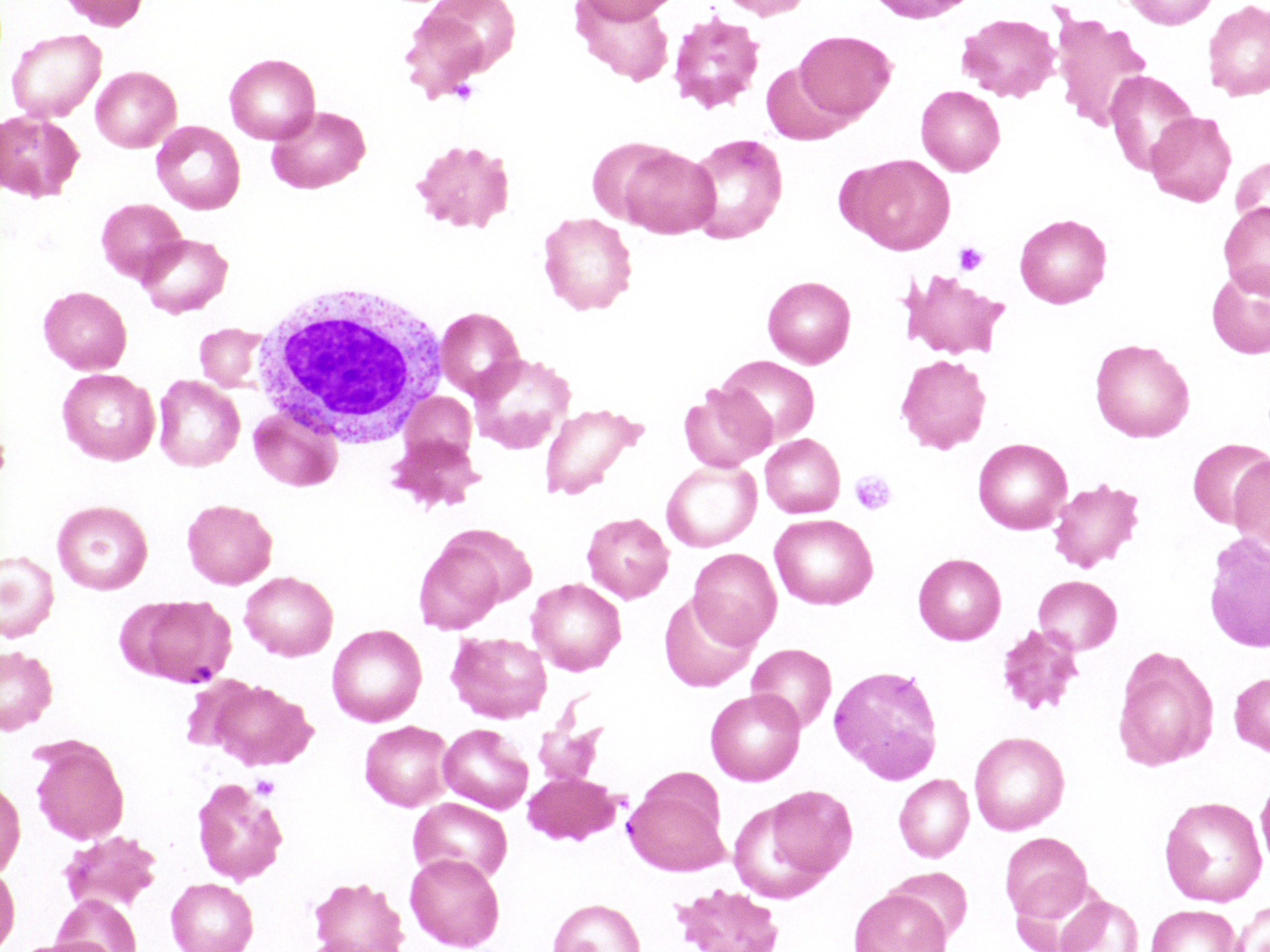
Case Presentation: A 76-year-old Chinese woman with history of cryptogenic cirrhosis (MELD-Na 25) presented to our hospital with 1 week of worsening jaundice, abdominal distension, and right upper quadrant pain. Cirrhosis was diagnosed by imaging on admission 2 months previously and presumed to be secondary to Hepatitis C infection due to antibody positivity. CT of the abdomen and pelvis at that time also demonstrated multiple small hyperattenuating liver masses. Subsequent multiphase CT of the liver demonstrated arterially enhancing lesions with persistent enhancement on portal and delayed phases. This was interpreted as progressive centripetal fill-in suggestive of hemangiomas. On examination, she was afebrile, diffusely icteric, and had mild abdominal distention. Initial labs revealed a total bilirubin of 17.5, with a direct component of 11.2. Hemoglobin was 10.1, decreased from 15.7 on prior admission. Follow-up CT was also interpreted as hemangiomas, although the lesions had markedly increased in size. A dominant left-hepatic lobe lesion again demonstrated avid circumferential enhancement with poor late-phase washout. Infection was ruled out as a cause of decompensation. Hepatitis C RNA PCR was not detected. During this admission, patient’s hemoglobin and platelets began to steadily decline. Blood smear showed immature forms and was also suggestive of a thrombotic microangiopathy. Bedside bone marrow biopsy was a dry tap. Liver biopsy ultimately yielded a diagnosis of hepatic angiosarcoma. However, two days later, patient rapidly decompensated. Hemoglobin decreased from 9.4 to 6.1, and platelets decreased from 111,000 to 63,000. Repeat blood smear showed evidence of a worsening microangiopathic process. Subsequent imaging showed an expansile perihepatic hematoma along the biopsy site. Total bilirubin continued to rise and was last measured at 42.6 on hospital day 17. On hospital day 18, she developed mucosal bleeding from the ears and mouth, which somewhat improved following administration of cryoprecipitate. Patient was made hospice care and went home with family.
Discussion: Angiosarcoma is a rare tumor representing less than less than 1% of all soft-tissue sarcomas and only 2% of all primary hepatic neoplasms. It is a rare but known cause of cirrhosis due to necrosis of hepatocytes secondary to massive tumor infiltration of hepatic sinusoids. As in our patient, it may present with a variety of clinical syndromes, including Kasabach-Merritt Syndrome (consumptive thrombocytopenia), myelofibrosis, and microangiopathic hemolytic anemia. On imaging, hepatic angiosarcoma can appear as multiple nodules (as in this case), a dominant mass, or a diffuse infiltrative lesion with variable enhancement patterns that can mimic hemangiomas, hepatocellular carcinoma, or metastases. Outcomes today remain poor regardless of whether patients present initially with localized or metastatic tumor burden, with a relapse rates as high as 40% reported in patients treated with primary surgical resection.
Conclusions: This case illustrates the need for a high index of suspicion when presented with a case of hepatic angiosarcoma, which may often be metastatic on presentation given its vascular origins and aggressive clinical course. Diagnosis of primary hepatic angiosarcoma is especially challenging given its predilection for early metastasis and frequent multisystemic involvement on presentation. Though imaging can be suggestive of malignancy, biopsy remains the gold standard for diagnosis.