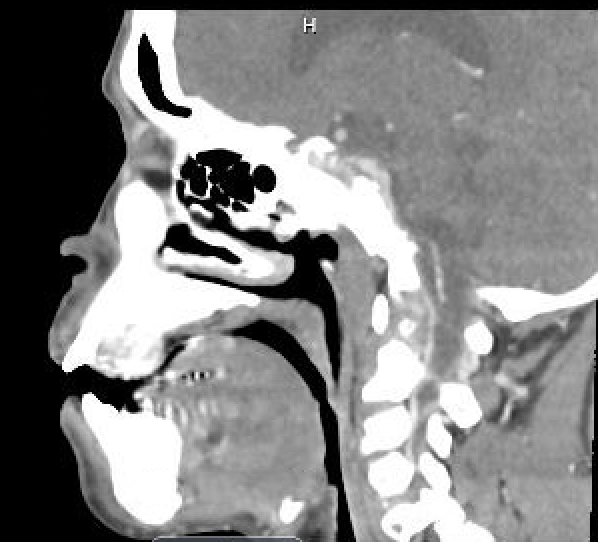
Case Presentation: A 48-year-old woman presented with a rapidly progressive brown tumor of the right anterior aspect of her hard palate. She had end stage renal disease for decades and secondary hyperparathyroidism for 16 years, which progressed to tertiary hyperparathyroidism within the past year. Two months prior to referral, she first noticed a lesion in her mouth. She presented to the Emergency Department a month later with progression of this lesion and pain radiating up the right side of her head. She reported difficulty breathing, speaking, eating, sleeping, and progressive hearing loss in the right ear. On physical exam, a firm, exophytic, nontender mass approximately 5 cm in diameter was seen on the right anterior aspect of the hard palate, causing malocclusion of the related teeth (Figure 1). A 1 cm right-sided submandibular lymph node was palpated. Laboratory findings were as follows: intact parathyroid hormone (PTH) 3,089 pg/mL (15-65 pg/mL), serum calcium 10.8 mg/dL (8.5-10.6 mg/dL), phosphorus 5.1 mg/dL (2.7-4.5 mg/dL), and alkaline phosphatase 1,098 U/L (35-140 U/L). A CT scan demonstrated a 2 cm circumscribed, hyperdense, enhancing mass arising from the right anterior hard palate projecting into the oral cavity (Figure 2). Repeat imaging one week later revealed tumor growth to 5 cm, and a biopsy revealed spindle and giant cells, consistent with a diagnosis of brown tumor. Surgical debulking of the brown tumor and subtotal parathyroidectomy were performed, revealing a parathyroid adenoma measuring 2.5 cm in diameter within the capsule of the left thyroid gland. PTH was monitored peri-operatively and decreased to 159 pg/mL. The patient’s post-operative course was complicated by severe hungry bone syndrome which required aggressive intravenous calcium repletion.
Discussion: Brown tumors are focal, bony lesions caused by increased osteoclastic activity and trabecular fibrosis due to hyperparathyroidism. They have become a rare entity in the developed world and are most commonly seen as an end-stage manifestation of primary hyperparathyroidism. To our knowledge, this is the first case of maxillary brown tumor to be reported in a patient with tertiary hyperparathyroidism in the United States. Localization of brown tumors to the maxilla is exceedingly rare and appears to be more common in females. With early diagnosis and treatment of hyperparathyroidism, the prognosis is excellent for most patients. However, there have been a few reported cases of tumors that failed to regress and became even larger after parathyroidectomy. While direct excision of the brown tumor is generally not recommended, it may be indicated for a lesion in a compromising anatomical site, as in our case, or a lesion that fails to regress after one to two years of follow-up.
Conclusions: In conclusion, we present an exceptional case of maxillary brown tumor associated with tertiary hyperparathyroidism in a 48-year-old woman, which presented with rapid growth and functional impairment. Brown tumors are uncommon today due to improvements in laboratory technology that allow earlier diagnosis and treatment of hyperparathyroidism. This case demonstrates several critical clinical points in managing brown tumor. Diagnosis requires clinical and laboratory evidence in addition to radiographic and histopathologic findings. Surgical resection of the brown tumor should be considered for certain anatomical sites and for refractory cases.