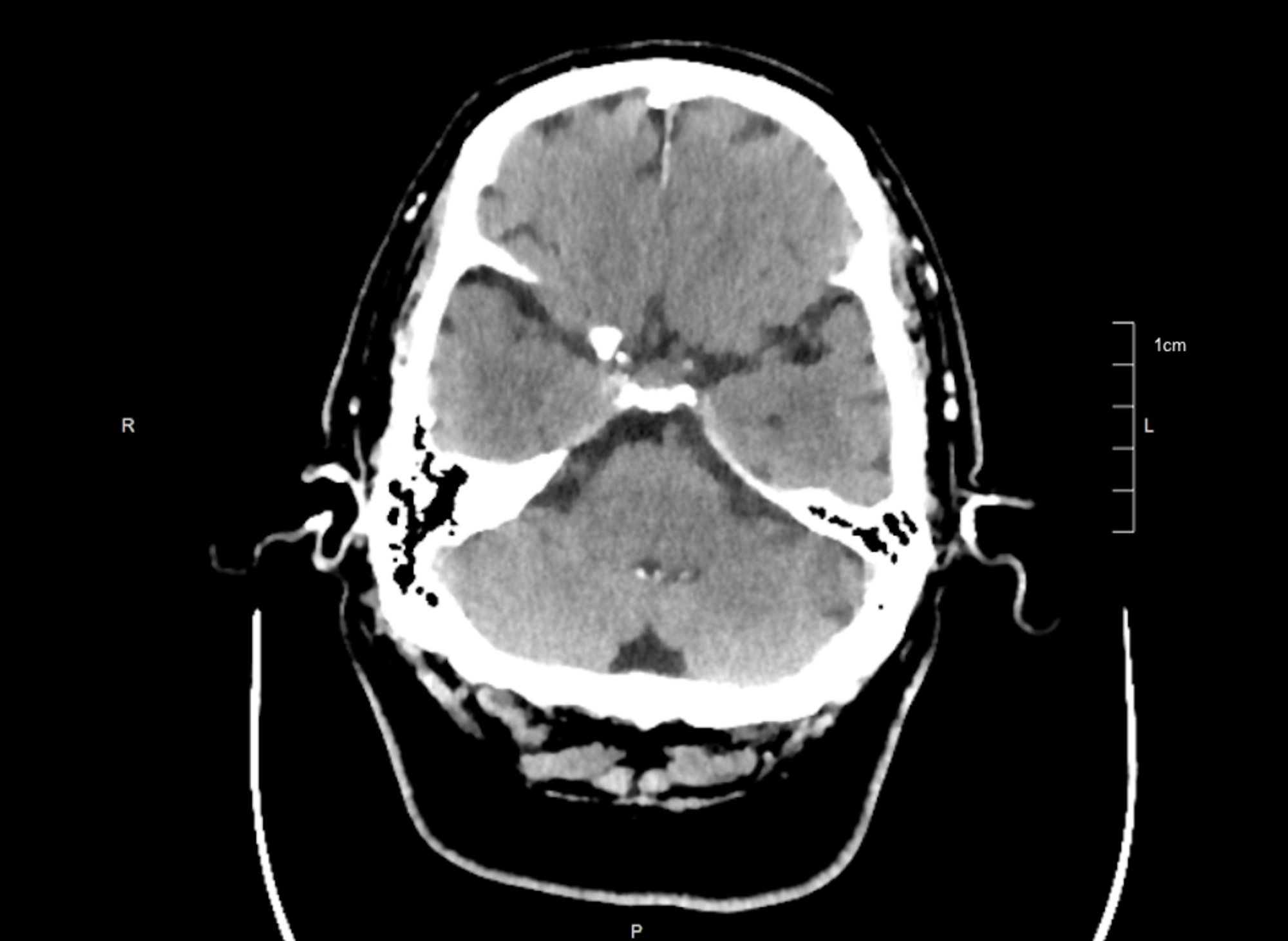
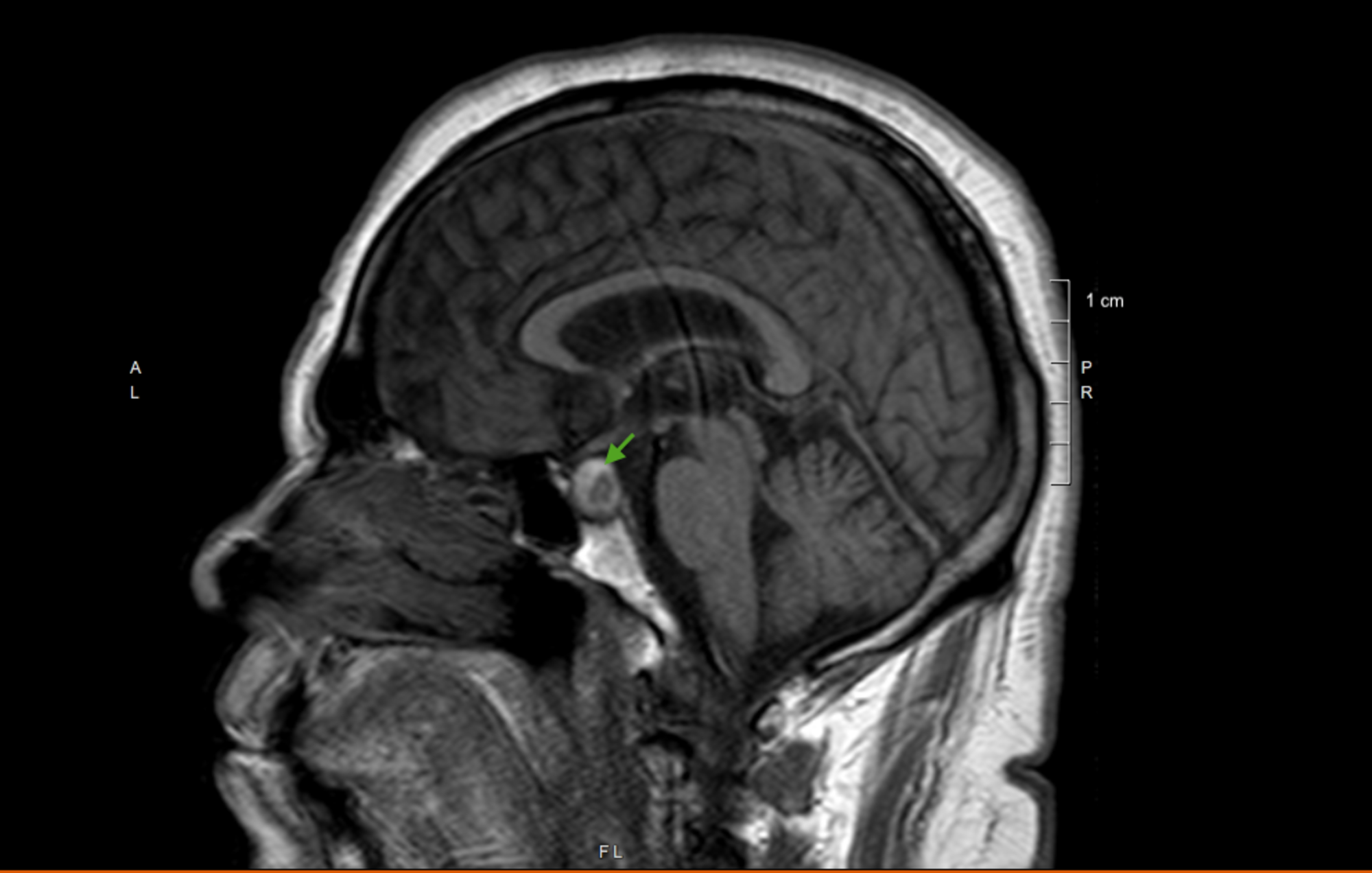
Case Presentation: A 73-year-old male with a medical history of hypertension presented with vomiting of 5 days. Vomitus was non-bloody, non-bilious in nature and was associated with headache. The headache was sudden in onset, bifrontal, 8/10 on a numerical rating pain scale.Initial vitals were remarkable for BP of 68/54 mm Hg which improved to 94/55 mm Hg after 2 L of saline infusion. Physical exam revealed dry mucosa with no evidence of focal neurological deficits. CT head was showed no evidence of acute intracranial pathology. Initial blood workup revealed hyponatremia with serum sodium of 128 mmol/L and serum potassium of 3.2 mmol/L. Blood urea nitrogen and serum creatinine were 56 mg/dL and 3.3 mg/dL respectively.The patient was admitted with an impression of acute kidney injury due to acute volume depletion resulting from vomiting. Aggressive hydration was initiated. Electrolytes were replaced. Over the next several hours, the hypotension resolved with the improvement in kidney function. However, the patient continued to report a persistent headache. 12-18 hours later, the patient developed a double vision with left-sided ptosis. MRI brain without contrast revealed a pituitary mass of 1.2 cm x 1.3 cm x 1.2 cm size, arising from the left side of the pituitary gland within the sella, which was peripherally hyperintense on the T1 image. Also noted was the rightward displacement of the pituitary stalk without displacement of the optic chiasm. Subsequent blood tests revealed an extremely low level of serum cortisol at 0.69 mcg/dl(N:4.46-22.7). TSH level was 0.3 mIU/ml and serum prolactin level was 2.6 ng/ml. Pituitary apoplexy was diagnosed and intravenous hydrocortisone was infused. Neurosurgery was consulted for immediate surgical decompression.
Discussion: Pituitary apoplexy (PA) is a rare medical condition, with an incidence of 0.17 episodes per 100,000 person-years[4]. PA occurs due to ischemia and infarction followed by hemorrhage when the pituitary tumor outgrows its blood supply[6]. Headache is the most common symptom reported in patients with PA followed by nausea and vomiting [1,9]. The origin of the headache is unclear but is thought to be due to meningeal irritation[9-10]. Hypotension seen in patients with PA is explained by the hypocortisolism resulting from the deficiency of adrenocorticotrophic hormone (ACTH).In this index patient, AKI resolved after rehydration and supportive care. However, the headache persisted. With the development of double vision, MRI brain was considered which was suggestive of pituitary apoplexy. Laboratory tests were confirmatory. As in our case, CT head is known to be less sensitive than MRI in diagnosing PA. MRI brain is superior to CT head in identifying pituitary tumors (100% vs 93%) and hemorrhage (88% vs 21%) and remains the gold standard in diagnosing PA[13,15-17].Hypotension is a well-documented risk factor for acute kidney injury. However, AKI is a less recognized complication in patients with PA. The likely mechanism of AKI in this patient is hypotension due to the deficiency of corticosteroids resulting from PA. Renal vasoconstriction in patients with hypotension and true volume depletion results in decreased renal perfusion and thereby decrease in the GFR.
Conclusions: Pituitary apoplexy presenting as acute kidney injury is rarely reported. A detailed history and evaluation by the clinicians with an emphasis on the etiologies of the presenting complaints are necessary to identify such medical emergencies. MRI is far superior to CT in diagnosing PA.