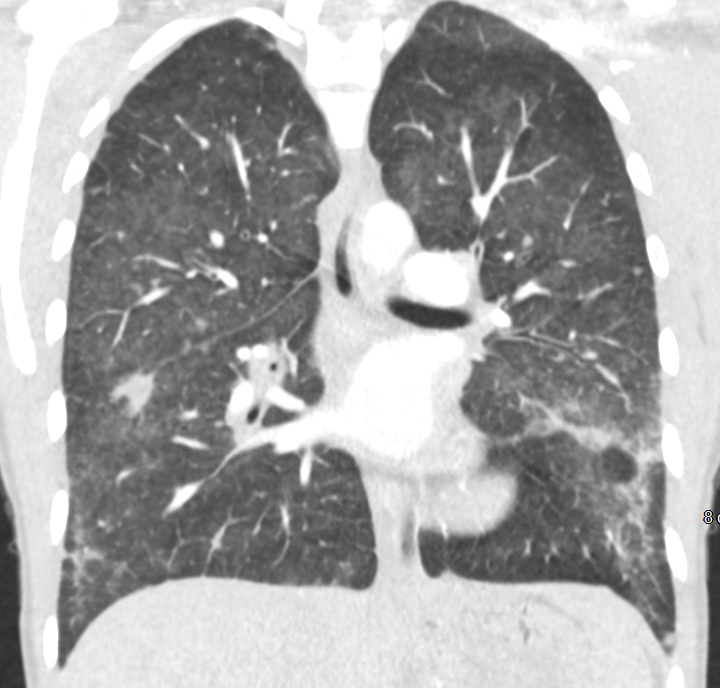
Case Presentation: A 25-year-old woman with history of childhood asthma presented with 1 week of fever, dry cough and chest discomfort. She also had non-bloody diarrhea, nausea and vomiting. On review, she admitted vaping THC and CBD products for the past 9 months. She was afebrile with HR 115 bpm, BP 130/61 mmHg, RR 18/min and SaO2 95% on room air. She was ill-appearing, tachycardic with regular rhythm and had mild rales heard in the lower lung fields. Lab findings revealed a leukocytosis of 16,800 WBC/ul with 91% neutrophils. Chest x-ray was normal, but chest CT showed multifocal ground glass opacities with tiny pleural effusions and no pulmonary embolism (figure 1). Nasopharyngeal respiratory pathogen PCR and urine streptococcus and legionella antigens were negative. HIV antibody was negative and BNP was normal. Sputum culture grew oral flora, and AFB and fungal smears were negative. PCR from stool was positive for enteroaggregative E. coli and IV azithromycin was started. Bronchoscopy was limited due to severe procedural coughing; however, infectious studies from aspirated fluid were negative. ANA, ANCA, RF, CCP, C3, and C4 were normal. A diagnosis of vaping-induced lung injury was favored and IV steroids were started.She clinically improved after 2 days. Prior serology studies returned with positive mycoplasma pneumoniae IgM and IgG antibodies. Immunofluorescence testing for M. pneumoniae IgM was also positive. Given these findings and the prior GI PCR, she completed 5 days of azithromycin and was discharged on a rapid steroid taper. Two weeks later, she reported near-resolution of her cough and had no GI or systemic symptoms.
Discussion: A form of acute lung injury related to the use of e-cigarettes, particularly those containing THC, has recently emerged. Presenting symptoms usually include cough, chest pain and shortness of breath, and frequently occur with concurrent abdominal pain, nausea, vomiting and diarrhea. Fever, chills and weight loss are also common. Chest exam is often unremarkable while chest x-ray may show pulmonary infiltrates or appear normal. Basilar-predominant consolidation and ground-glass opacities, with lobular or subpleural sparing, are often seen on CT. However, these same symptoms and findings are also found in other acute illnesses such as typical and atypical bacterial pneumonias, viral infections, endemic mycoses and opportunistic infections. This patient’s GI symptoms were likely due to E. coli enterocolitis. The initial respiratory PCR was negative for mycoplasma perhaps due to sampling only from the upper respiratory tract or the early disappearance of M. pneumoniae as a result of her immune response. Mycoplasma pneumonia is preferably diagnosed using serology combined with direct pathogen detection. If discordant, a significant rise in specific antibodies over time may more accurately provide evidence of active infection. Whether vaping synergistically worsens mycoplasma or other common pulmonary and/or GI illnesses is unknown.
Conclusions: Although vaping-induced lung injury has become an epidemic among users of e-cigarette products, this remains a diagnosis of exclusion. Alternate etiologies of acute pulmonary and GI illness must be ruled out, particularly pulmonary mycoplasma infection. Empiric treatment for pneumonia when vaping-induced injury is suspected appears prudent. As in this case, hospitalists should be mindful of availability heuristic and anchoring bias when considering vaping-induced lung injury.