Case Presentation: A 35-year female presented to the ED with complaints of worsening abdominal pain and distension without nausea, vomiting or diarrhea. The abdominal pain was diffuse in nature without radiation. She had fatigue, chills, intermittent fevers, and 10 pounds of weight loss over a month. The review of systems was otherwise negative. She was afebrile, with normal vitals. Physical exam was significant abdominal distension with fluid wave present and diffuse abdominal tenderness. The reminder of her exam was unremarkable.Further history revealed that she recently immigrated from Afghanistan 4 years prior. She had prior admission one month ago for similar complaints. Computed tomography (CT) scan revealed a multiloculated cystic left adnexal mass that measured 7.1 x 4.3 cm in size with evidence of ascites and extensive peritoneal studding. CT scan of the chest showed 2 right lower lobe lung nodules with calcified hilar lymph nodes. A paracentesis was performed and sent for cytological analysis which was negative for malignancy. Additionally, an omental biopsy obtained yielded predominantly non-necrotizing epithelioid granulomas with lymphohistiocytic reaction without signs of malignancy. Other labs from this prior visit were significant for a CA 125 elevated to 1664 U/mL (0,0-35.0 U/mL). Acid-fast bacillus (AFB) staining at the time was negative and the fluid was sent for mycobacterium culture. Repeat paracentesis this admission revealed 1890 nucleated cells, 1100 RBCs, 30 polymorphic neutrophils, SAAG <1.1 and elevated adenosine deaminase (ADA) 8.1 U/L(0.0 to 7.3 U/L). Interferon-gamma release assay was positive and all other obtained cultures remained negative. With positive ADA and geographic risk factors, the patient was started on rifampin, isoniazid, pyrazinamide, and ethambutol. She was placed in airborne isolation which was discontinued after determining negative pulmonary TB work up. Two weeks after discharge, her original mycobacterium culture from the first paracentesis grew M.tuberculosis complex confirming the diagnosis. Her abdominal pain and distension significantly subsided thereafter, and repeated ultrasound of the abdomen showed a reduction in ascites volume. The patient continued on anti-tuberculosis therapy.
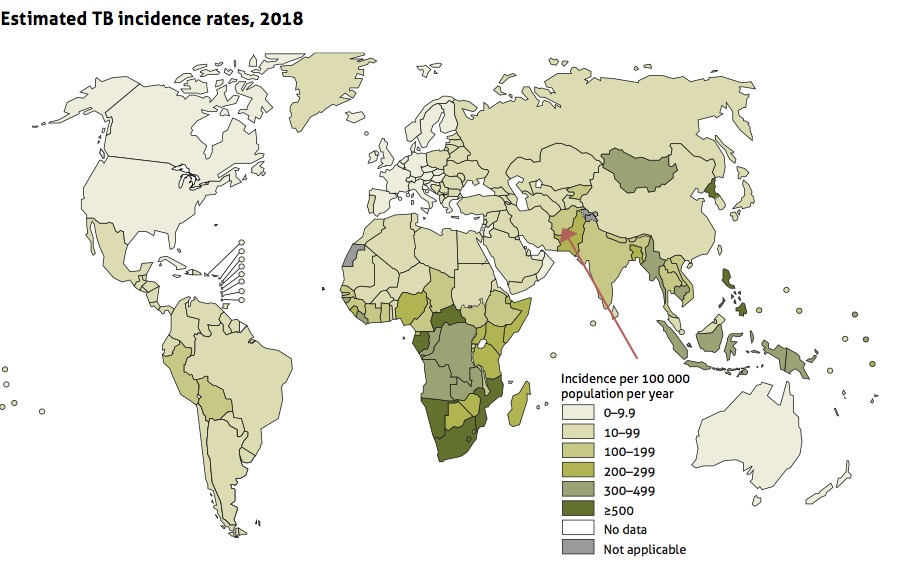
Discussion: This patient represents an important case of undifferentiated abdominal pain and ascites. Differentials considered included ovarian malignancy, cirrhosis, sarcoidosis, and peritoneal TB. Peritoneal TB is a rare manifestation of the infection, representing 5% of all cases of TB globally. It should be considered in the differential for those from endemic areas that include Sub-Saharan Africa and areas of the Middle East including Afghanistan. This case is particularly important as it mimicked a metastatic ovarian malignancy with the constellation of cystic ovarian mass, ascites with peritoneal studding, distal lung nodules and an elevated CA-125. Interestingly, CA-125 levels were found to be a useful marker in differentiating pulmonary tuberculosis from other infections.
Conclusions: Peritoneal TB is an important etiology of ascites in individuals from endemic TB areas. In female populations, it can mimic the appearance of ovarian malignancy. Prompt recognition is vital from a public health standpoint to rule out active TB and for early initiation of treatment.