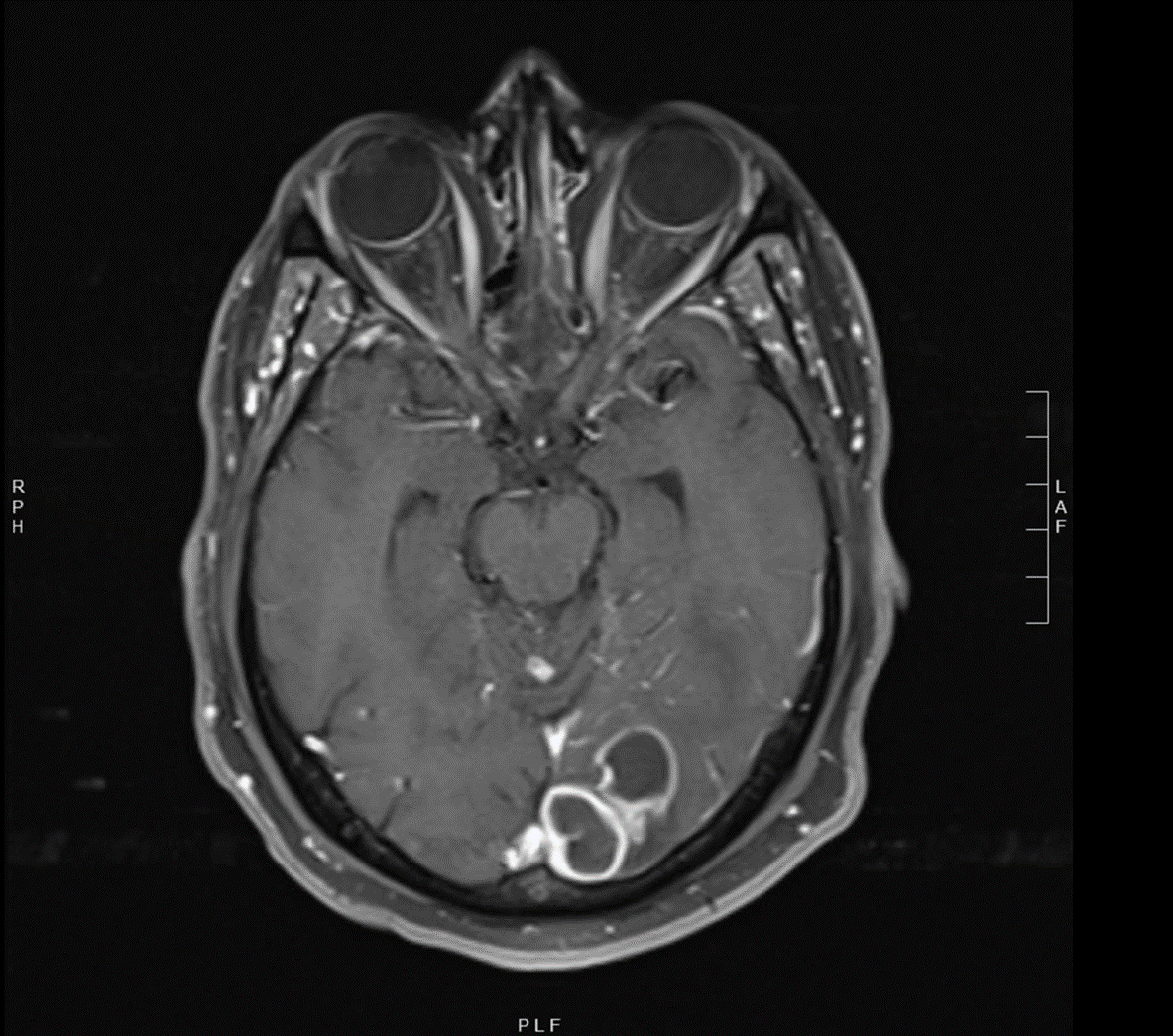
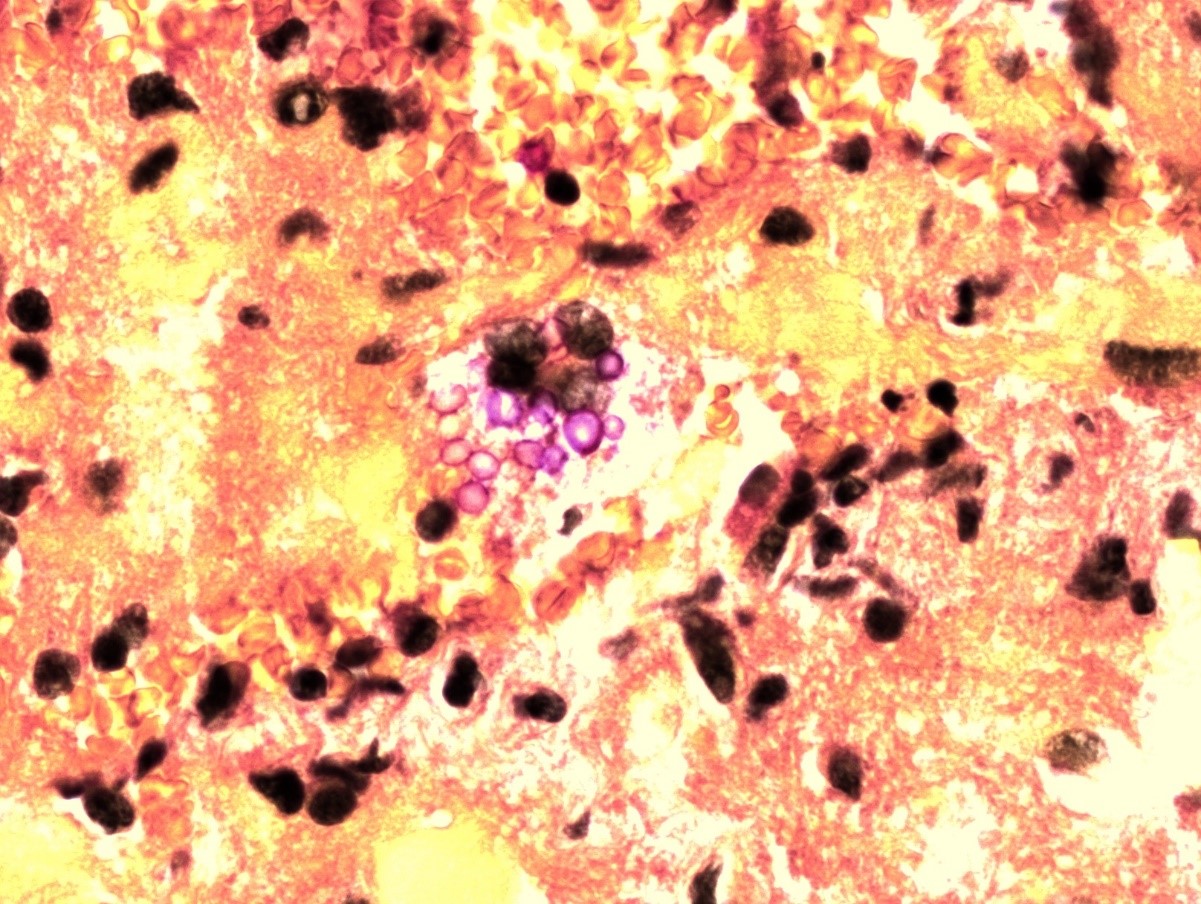
Case Presentation: 50 y.o African American male with a history of schizophrenia presented for headache, blurred vision and acute onset aphasia. On exam, patient was alert, but unable to follow commands. He was noted to have poor dentition. Lab studies revealed WBC count of 4.1 with 47% neutrophils. BMP and liver function studies were unremarkable. Urine drug screen and alcohol levels were negative. TSH and vitamin B12 were normal. T. pallidum IgG and RPR were reactive with 1:2 titer. HIV and hepatitis panel were negative. Head CT revealed a large amount of edema in the left posterior cerebral hemisphere involving occipital and posterior temporal lobes with underlying 2×2 cm hypodense mass. A brain MRI with and without contrast demonstrated a 4 x 2 cm cystic mass in the left occipital lobe. Patient was started on steroids plus ceftriaxone and metronidazole for a possible odontogenic abscess as dental imaging revealed periapical lucency of the left mandibular molar. No neurologic intervention was planned and patient underwent many tooth extractions. Transthoracic echo showed no vegetations. Mental status returned to baseline and aphasia resolved. After 1 week of treatment patient developed seizures and worsening confusion with labile mood. Due to concern for fungal disease, fluconazole was added and steroids were weaned. Further work up included negative serum cryptococcal antigen, blood and AFB cultures. Repeat MRI showed clustered ring-enhancing masses with mild progression. Patient was started on meropenem for enhanced CNS penetration, but continued to have confusion. LP was not initially performed due to concern for complications from increased intracranial pressure. Neurosurgery performed stereotactic brain biopsy of three cysts, one with a significant amount of purulence. Pathology with GMS silver and mucicarmine staining was consistent with Cryptococcus, and fungal cultures grew C. neoformans. Induction therapy with amphotericin B and flucytosine was initiated. Patient had persistent headache post-operatively and a lumbar puncture revealed opening pressure of 23 cm H20, no WBC, elevated protein, and a CSF crypto ag 1:40. India ink was negative. On repeat MRI imaging 3 months later patient had resolution of abscess. His repeat CSF showed no evidence of infection.
Discussion: Cryptococcus is the most common fungus to cause CNS manifestations. There are two known pathologic types in humans, C. neoformans and C. gatti. CNS involvement suggests dissemination and typically occurs in individuals with history of HIV or other immunocompromising condition. Cryptococcomas are rare and frequently misdiagnosed. Our patient was initially treated with broad-spectrum antibiotics for a presumed CNS odontogenic abscess. When repeat MRI showed progression of the mass, he underwent brain biopsy which confirmed C. neoformans cerebral cryptococcoma. On follow up after treatment with amphotericin and flucytosine, followed by maintenance fluconazole, he had clinically improved and repeat imaging showed abscess resolution.
Conclusions: This case highlights that cryptococcoma should be on the differential for immunocompetent patients with brain abscess despite negative cryptococcal antigen in serum. This is important to help avoid misdiagnosis and delayed treatment. A brain abscess >2.5 cm is an indication for surgical aspiration. If cryptococcomas are isolated, a search for underlying immunosuppression should be considered. In our patient’s case, an extensive work-up revealed diabetes, having a HbA1c of 8.2%.