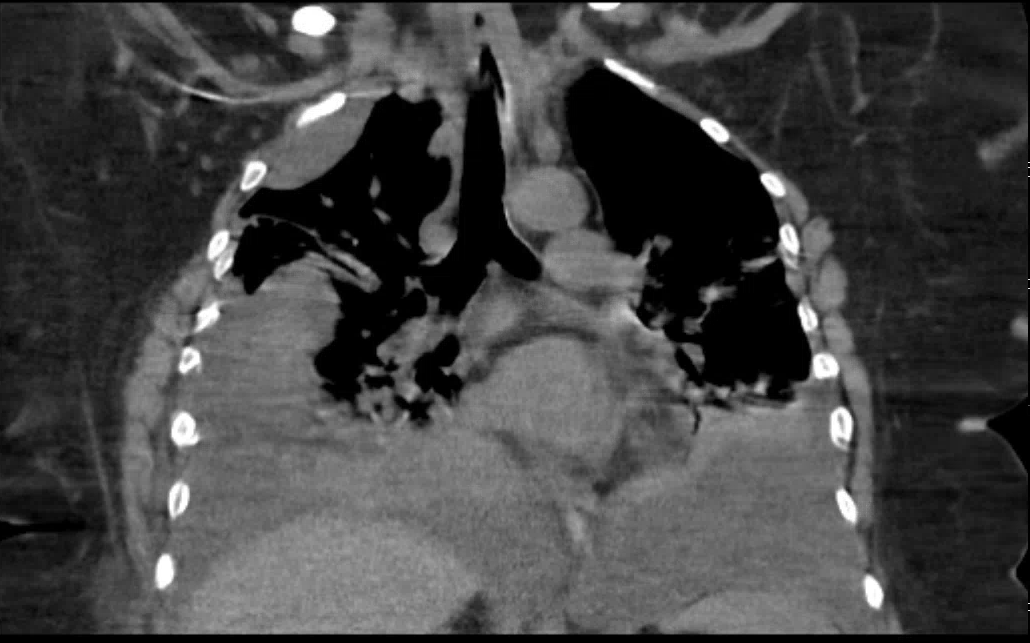
Case Presentation: A 60-year-old woman with a history of diabetes, hypertension, and sleep apnea presented to the hospital with acute onset shortness of breath. Several months prior, she had undergone dental extraction that was complicated by poor wound healing. Unusually, the surgeon noted pus from the site of extraction but when further analyzed, it was found to be lymphatic drainage. A sample was sent of her mandible and returned with pathology showing fibromyxoid connective tissue with myofibroblastic and vascular proliferative tissue noting massive osteolysis, suggestive of Gorham-Stout Disease (GSD), also known as ‘Vanishing Bone Disease’. Mandibular resection with reconstruction was performed due to pathologic fracture of the left mandible. Several weeks later, she presented with dyspnea and hypoxia. A CT thorax discovered large bilateral pleural effusions and pigtail catheters were placed with return of chylous fluid. At that time, cultures and cytology from the pleural fluid were negative. She then developed an exam suggestive of unilateral cervical myelopathy with CT C-spine showing extensive erosion of the clivus and C1 vertebrae causing dislocation and basilar displacement of the medulla. She underwent a bone scan showing additional involvement of the manubrium and left lateral skull. Multiple medical and surgical subspecialties worked together to formulate a treatment plan. Once her spine was stabilized, she was initiated on Sirolimus based on literature that supports the use of this treatment. Despite escalating doses, she continued to have high output from her chest tubes and she ultimately developed shock and respiratory failure requiring intubation and ICU care. In accordance with her wishes and continued deteriorating clinical status, the patient and family decided to pursue comfort measures and the patient expired after three months of hospitalization.
Discussion: GSD is a rare disease of unclear etiology characterized by proliferation of lymphatic endothelium causing massive osteolysis and bone resorption. It typically involves the skull, shoulder, pelvis and vertebrae, and affects children and young adults with the reported age range from 9 months to 49 years old (mean 18 years). Chylothorax is a severe complication noted in 17% of cases leading to progressive respiratory failure with a mortality rate exceeding 50%. The proposed mechanism behind the development of chylothorax is the direct extension of lymphangiectasia into the pleural cavity, or by the invasion of the thoracic duct due to involvement of adjacent thoracic spine. There are several proposed treatments, however, GSD typically responds poorly to therapies. Our case is unusual in that GSD was diagnosed in the sixth decade of life. Moreover, she developed bilateral chylothorax without thoracic spine involvement, conflicting with the proposed mechanism.
Conclusions: GSD represents a diagnostic and management challenge due to the paucity of knowledge surrounding its etiology and management. It is important for hospitalists managing these patients to understand that the care of these patients requires multidisciplinary coordination and input due to the rarity, unique clinical characteristics, lack of standard treatment, and high risk of mortality. It is also important to note its high mortality when associated with chylothorax, as it may lead to earlier enrollment in palliative services thus allowing patient to avoid unnecessary and burdensome health care.