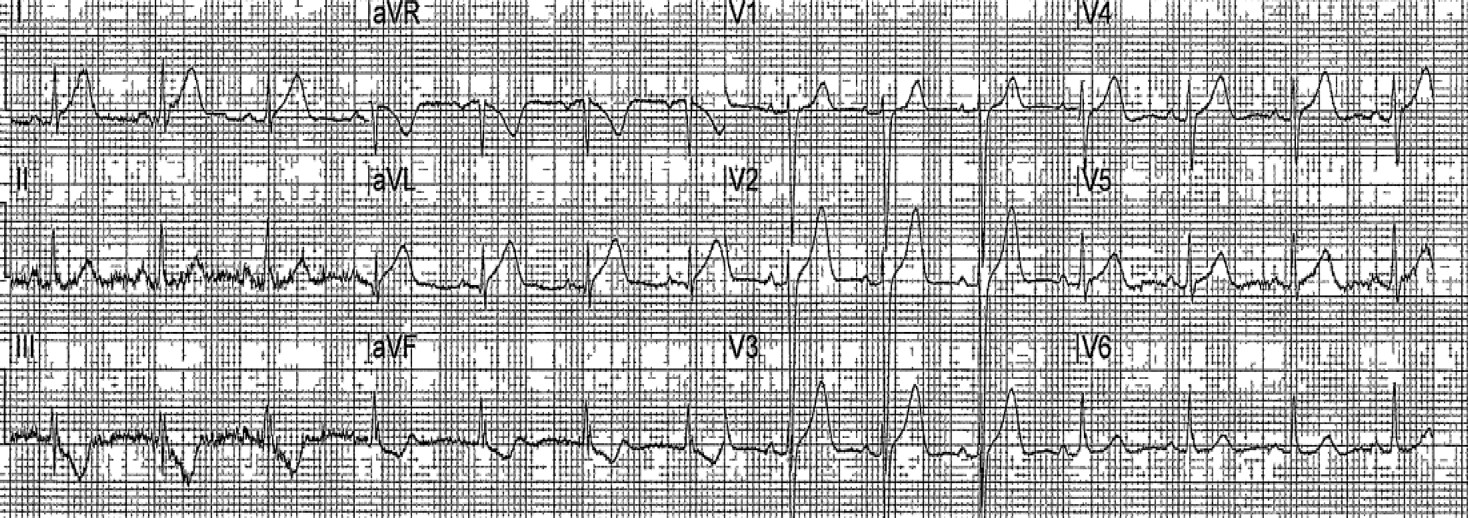
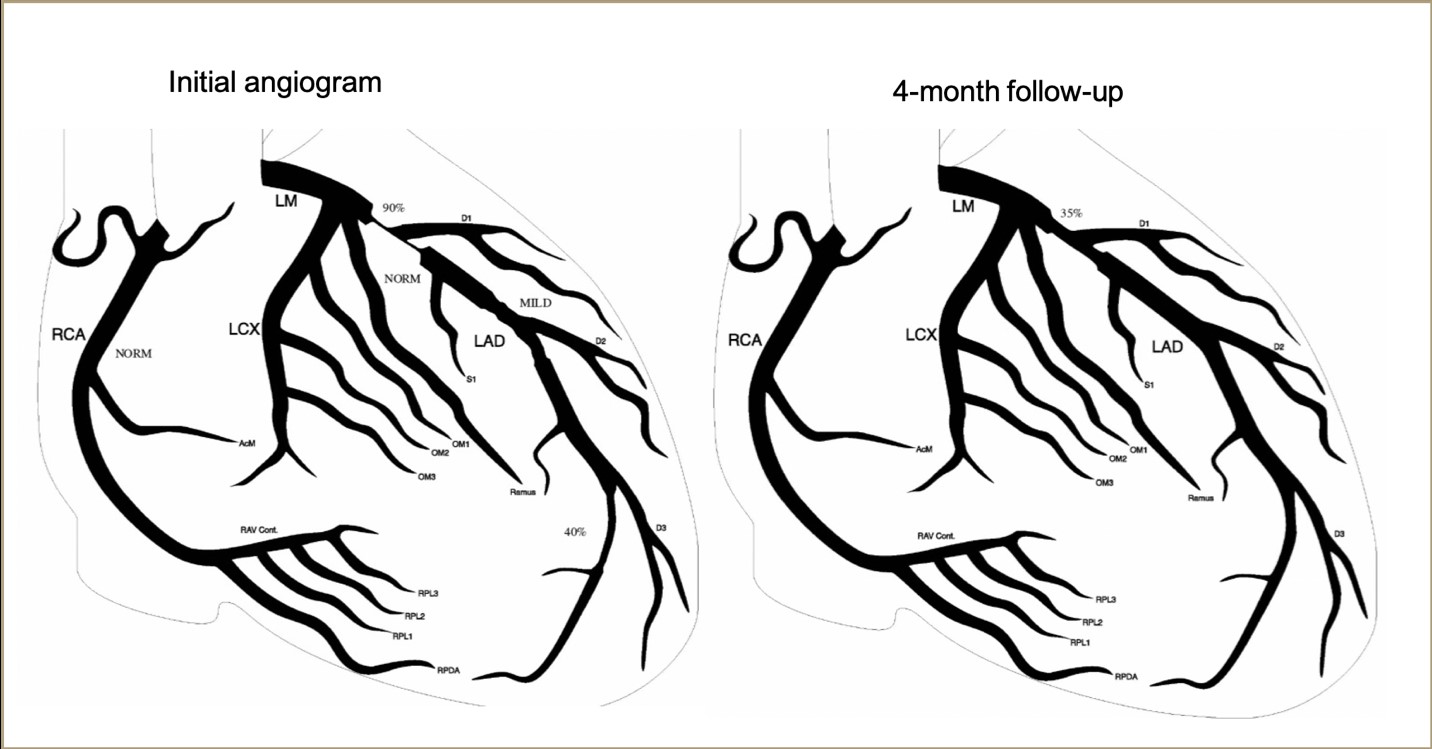
Case Presentation: A 33-year-old male presented to the emergency department (ED) after abrupt onset left anterior chest pain with associated diaphoresis, nausea, and abdominal pain one hour prior to arrival. He denied aggravating or relieving factors. Vital signs were stable and physical exam, including cardiac and respiratory exam, were unremarkable. Patient denied a history of heart disease, dyslipidemia, smoking, or illicit substance use. He also denied a family history of cardiac disease or fibromuscular dysplasia, though his mother did report a biological cousin that had spontaneous coronary artery dissection (SCAD) diagnosed at age 31. Electrocardiogram (EKG) in route to the hospital had ST elevation in lateral and inferior leads consistent with a STEMI (see figure 1), though repeat EKG in the ED revealed that the elevations had subsided and the patient’s pain had improved. Troponin in the ER was found to be 0.22 ng/ml. Patient underwent an emergent diagnostic angiogram which showed an angiographically normal left main coronary artery, a normal but tortuous dominant right coronary artery (RCA), and a medium sized left circumflex (LCx). There was a hazy narrowing of the proximal left anterior descending artery (LAD) as well as separate tubular area of the distal (LAD) which had angiographic appearance of SCAD. Patient was medically managed with heparin, tirofiban, nitroglycerin infusions, aspirin and high-intensity statin. Repeat angiogram 48 hours later showed healing lesions in proximal and distal LAD. Proximal LAD (previously 90% narrowed) was 40-50% narrowed and distal LAD segment was only mildly narrowed. Patient was discharged on duel antiplatelet (DAP) therapy and an angiogram was done 4 months later that showed healing of the proximal LAD, with no more than 30-40% residual narrowing, and complete healing of the distal LAD (see figure 2). Optical coherence tomography showed a focal intramural hematoma and complete absence of any atherosclerosis.
Discussion: SCAD is an important cause of myocardial infarction in those without traditional atherosclerotic risk factors. It is a non-traumatic, non-iatrogenic separation of the artery wall thought to be caused by an intimal tear or a vasa vasorum bleed. As the false lumen expands, it exerts a pressure on the true lumen causing ischemia. SCAD typically occurs in younger patients and women who are pregnant or postpartum [1], though it may also occur in people with predisposing factors such as fibromuscular dysplasia [2, 3].Dissections can be diagnosed by angiogram and can be treated in different ways including conservative therapy, percutaneous coronary intervention (PCI), coronary artery bypass grafting (CABG), and fibrinolytic therapy [2]. Though there are currently no guidelines regarding treatment, many cases are treated with medical management which generally includes DAP, beta blockade, and statins [4]. Those patients who present with infarction, ongoing ischemia, or hemodynamic comprise are recommended to be considered for revascularization with PCI or CABG.
Conclusions: SCAD is a rare cause of myocardial ischemia in patients without a history of atherosclerotic risk factors and can be diagnosed by angiogram. It can be medically managed using heparin, beta blockers, antiplatelet therapy and statins in patients that are hemodynamically stable. In patients that cannot be medically managed, PCI or CABG should be considered.