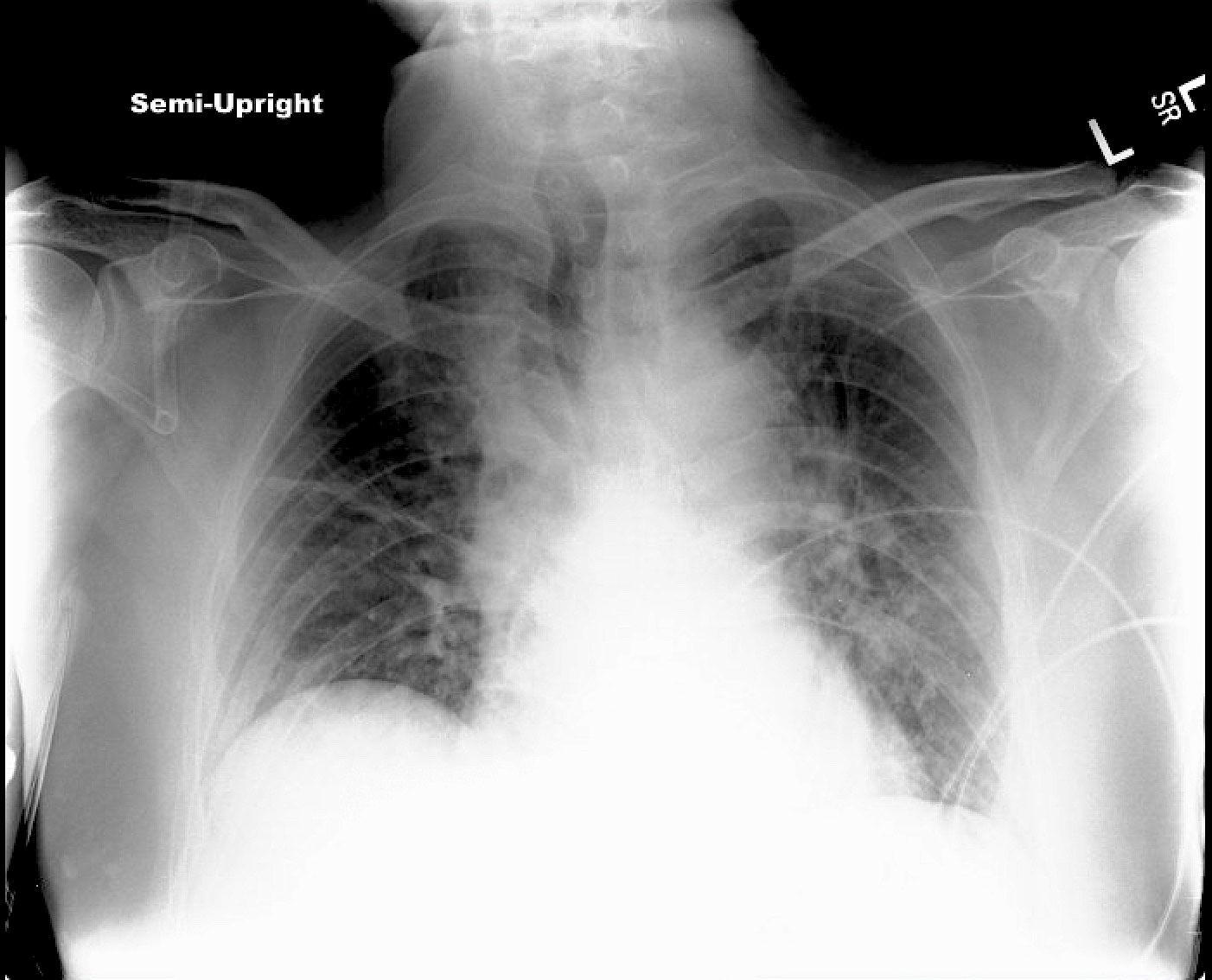
Case Presentation: A 56 year-old man with heart failure with preserved ejection fraction, aphasia and right-sided weakness from prior strokes presented with two days of difficulty with speech and ambulation. His vital signs were normal except for an oxygen (O2) saturation of 94% on 6 liters. On exam he was somnolent but able to follow basic commands. His lungs were clear bilaterally. He had no heart murmurs or gallops and his JVP was not elevated. He had no lower extremity edema. He had a mild leukocytosis, an elevated hematocrit (Hct) of 65.5%, and an MCV of 77 fL with a low iron level. CT angiogram of his head/neck revealed bilateral ischemic strokes in watershed territories and severe bilateral carotid disease. He was admitted to a surgical service for management of carotid stenosis.The medicine service was consulted for hypoxia. A CXR and CT pulmonary embolism (PE) protocol were obtained which revealed interstitial opacities compatible with pulmonary edema. He was diuresed with furosemide, but despite large urine output and net negative fluid balance, his oxygen requirement increased to 20 liters over the next two days. Repeat CXR demonstrated hazy perihilar opacities consistent with unchanged pulmonary edema. A brain natriuretic peptide (BNP) was 16 pg/mL and Hct was 66.8%. Given growing concern for hyperviscosity, his imaging was reviewed with radiology, who confirmed volume overload and hyperviscosity due to polycythemia would appear similar on chest imaging. He was given 1 liter of normal saline with improvement in his O2 requirement to 6 liters and Hct to 64.8%. An erythropoietin (EPO) level was low at 3.2 IU/L; JAK2 testing showed a V617F mutation, confirming a diagnosis of polycythemia vera. Hydroxyurea was started and he underwent daily therapeutic phlebotomy with plans to begin aspirin post-operatively.
Discussion: Absolute polycythemia – increased peripheral RBC mass (Hct >49% for men, >48% for women) not from hemoconcentration – is a common finding in hospitalized patients but is rarely the primary reason for admission. Secondary or reactive polycythemia is due to an elevated EPO level, found in patients with chronic hypoxia (heart failure, chronic obstructive pulmonary disease, obstructive sleep apnea), residence at high altitude, high O2-affinity hemoglobinopathies, and rarely EPO-secreting tumors. Primary polycythemia, or polycythemia vera (PV), is a myeloproliferative neoplasm arising from an activating JAK2 mutation in RBC progenitor cells. EPO levels are appropriately suppressed and a JAK2 mutation is often present. PV is associated with an increased risk of both venous and arterial thrombosis. Significant elevations in RBC mass lead to complications from blood hyperviscosity, including hypoxia and decreased cerebral perfusion. Chest imaging can show perihilar congestion that mimics pulmonary edema, but blood viscosity and hypoxia worsen with diuresis. PV is treated with correction of dehydration, phlebotomy to a Hct target of <45%, aspirin, and cytoreductive therapy (often hydroxyurea) in high-risk cases.
Conclusions: Hospitalists should have a high suspicion for PV in euvolemic patients with an elevated RBC mass and low EPO level, with or without evidence of thrombosis. Patients with PV may display signs of hyperviscosity, including hypoxia, that can be mistaken for common clinical comorbidities like heart failure. Chest imaging may also be misleading. Treatment to a goal Hct <45% decreases thrombotic complications and is critical peri-operatively to optimize surgical risk.