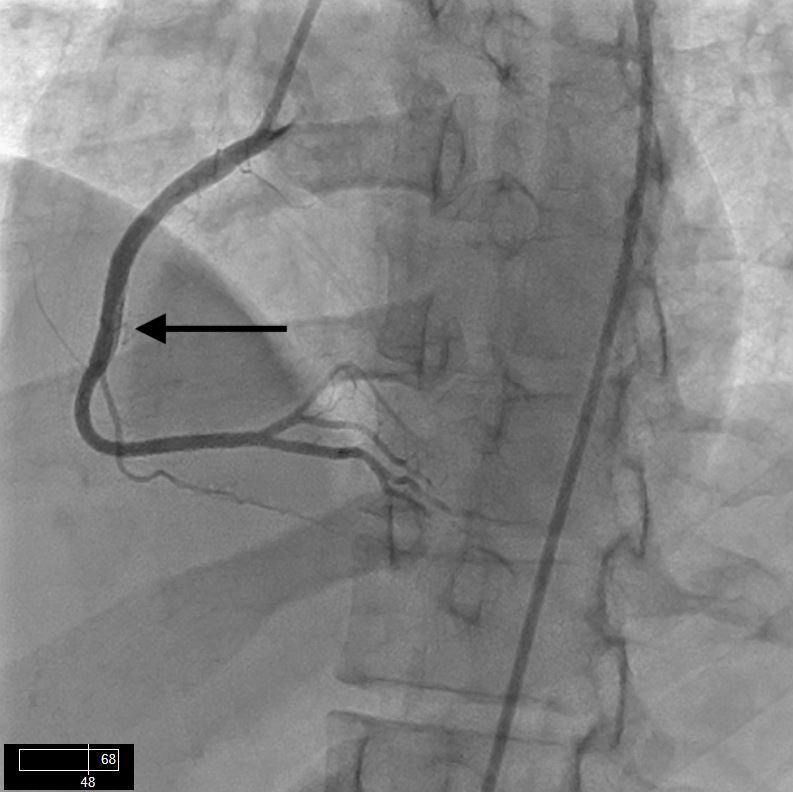
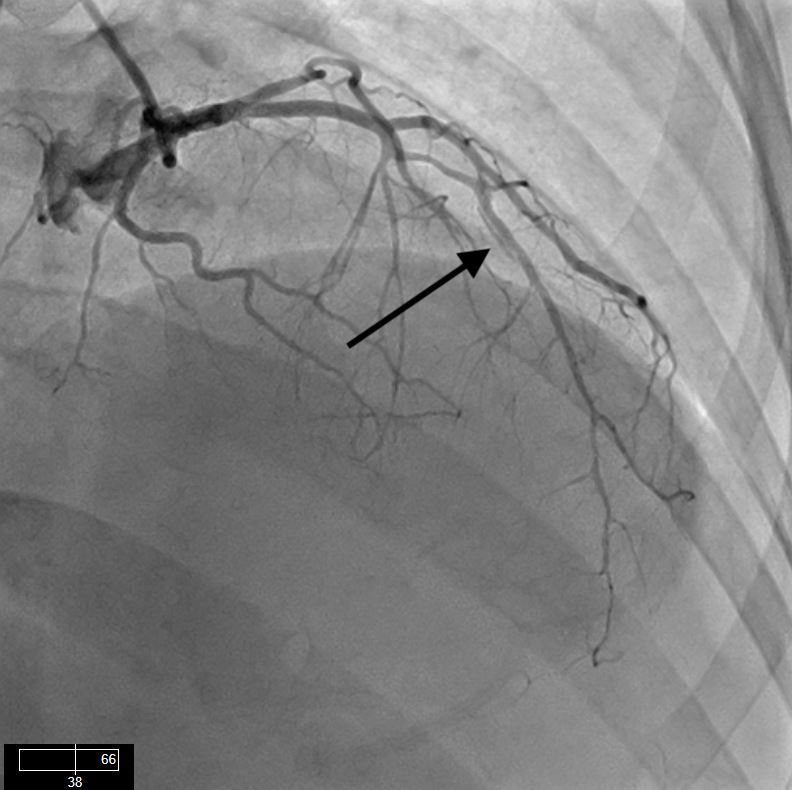
Case Presentation: Spontaneous coronary artery disease (SCAD)—an uncommon cause of coronary syndrome and sudden cardiac death—has been studied and described in greater detail in recent years. However, it still represents a diagnostic challenge with a high degree of uncertainty for proper management.A 37-year-old Hispanic female presented to the emergency department at another facility for sudden excruciating substernal chest pain associated with sweating, tingling, and numbness in the upper extremities. Although she is a heavy tobacco user, the patient has no history of hypertension, diabetes, or dyslipidemia, and her last delivery was more than one year ago. The patient’s physical examination was unremarkable, and her blood pressure was not significantly different between the right and left arms. The initial ECG did not show ST-T changes concerning for acute coronary syndrome. Laboratory tests were normal, including the first set of troponins. The second set of troponins was found to be elevated to 3.0, and the patient was started on aspirin, metoprolol, morphine, and a therapeutic dose of enoxaparin and subsequently transferred to our PCI capable facility. The patient underwent left heart catheterization, which showed preserved left ventricular function with mild anteroseptal hypokinesis, and a very distal left anterior descending artery with total occlusion at the apex. The patient was medically managed. After 48 hours of observation, the patient was pain-free with no new events. She was discharged home with secondary prevention medical therapy. On the third day after discharge, the patient returned to the emergency department with acute severe constant right-sided chest pain. Physical examination was remarkable, resulting in diagnoses of hypotension and tachycardia. The initial electrocardiogram showed 1.5 mm ST-segment elevation in leads II, III, and AVF. Laboratory tests showed elevated troponin to 6.0. Acute coronary syndrome treatment was administered to the patient.Another coronary angiography was performed, which revealed spontaneous dissection of the mid-left anterior descending artery (LAD) and mid-right coronary artery that were not present in previous cardiac catheterization. After angiography, patient became hypotensive with significantly elevated ST segments on monitoring, and an aortic balloon pump was placed. Cardiothoracic surgeons were consulted emergently for a coronary artery bypass. The patient underwent a successful CABG with venous bypass to the right coronary and left descending. She clinically improved after 5 days post-surgery and was discharged home with continuous medical therapy.
Discussion: Spontaneous coronary dissection can be a sudden and catastrophic condition. The majority of cases occur in a population with minimal or no risk factors for cardiovascular events, decreasing the immediate diagnosis of acute coronary syndrome. Recommendations for treating this condition vary from expectant management to emergent bypass surgery.
Conclusions: Additional efforts should be made to increase awareness and recognition of this condition as well as to collect more data to identify proper diagnostic techniques and procedures.