Background: Medical short stay units (SSU) are increasing in prevalence and frequently care for patients with infections. Antibiotic misuse at discharge from acute hospitalization is common. SSUs, which have rapid patient turnover, could have increased risk for antibiotic misuse during care transitions. Thus, we aimed to characterize antibiotic misuse at discharge from SSUs.
Methods: We conducted a retrospective cohort study of 100 adult patients discharged on oral antibiotics for common infectious conditions between May 2018 and September 2019 from two SSUs at a single center. Notably, this center has robust inpatient antibiotic stewardship with high performance on antibiotic use measures, but no interventions targeting either SSU. Through independent case review by two reviewers, we characterized antibiotic regimens as appropriate vs. misuse (antibiotic use where potential for harm exceeds possible benefit) according to hospital (and national) guidelines. Discrepancies in misuse classification were resolved by a third reviewer. Misuse included antibiotic overuse (unnecessary use, excess duration, or avoidable fluoroquinolone use) and guideline discordant use (suboptimal or inappropriate antibiotic selection). Variables associated with misuse were identified using Chi-squared, Fisher exact, or two-sided t-tests, as appropriate. In addition, we report odds ratios, adjusted for patient characteristics, to evaluate whether antibiotic misuse after discharge was associated with patient outcomes.
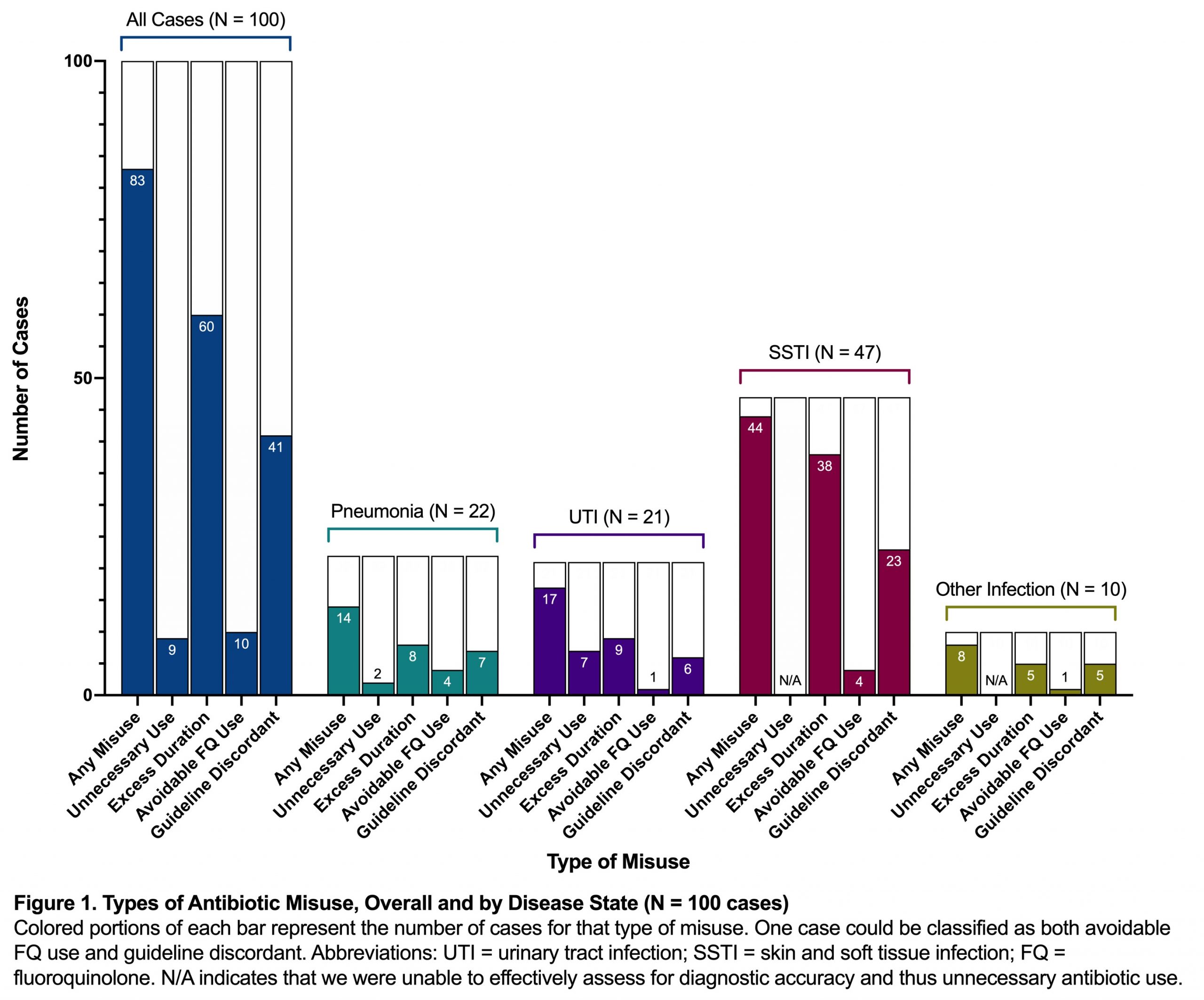
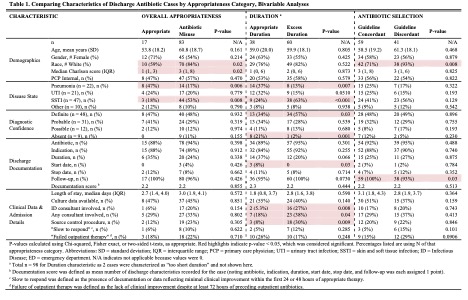
Results: Of antibiotic regimens prescribed at discharge, 83% (83/100) involved antibiotic misuse, including 94% (44/47) of skin and soft tissue infections (SSTI), 81% (17/21) of urinary tract infections (UTI), and 64% (14/22) of pneumonias. The most common types of antibiotic misuse were excess duration (60/100) and guideline discordant selection (41/100). SSTIs were most associated with misuse, accounting for 63% (38/60) of excess duration cases and 56% (23/41) of guideline discordant selection cases. Potential factors influencing antibiotic prescribing included consultant involvement which was present in 32 cases of which 84% (27/32) had antibiotic misuse, including 95% (19/20) of SSTIs. A diagnosis of SSTI (p<0.001), higher diagnostic certainty (p=0.03), any consult (p=0.04), an ID consult specifically (p=0.008), and requiring a source control procedure (p=0.009) were all associated with excess duration. There was no difference in outcomes between patients who had appropriate antibiotics vs. antibiotic misuse at discharge though there was a trend toward higher 90-day readmissions in patients receiving excess duration vs. appropriate duration (adjusted OR 3.57, 95% CI 1.00 – 12.83).
Conclusions: Despite inpatient stewardship efforts, substantial antibiotic misuse occurs at discharge from SSUs. Antibiotic stewardship interventions focused on SSUs are needed to improve discharge prescribing practices; key targets include antibiotic duration and the management of SSTIs.