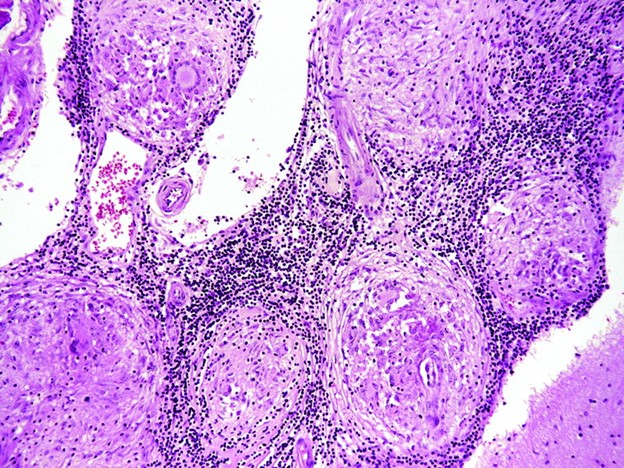
Case Presentation: This is a 65 y.o. male with PMHx significant for Monoclonal Gammopathy of Undetermined Significance (with prior negative skeletal survey and negative bone marrow biopsy), CKD stage III who presented with chief complaint of lethargy, bilateral extremity weakness, and dysarthria. Patient stated that he has been experiencing such symptoms for the past year, with acute worsening of symptoms over the last three weeks. Physical exam was notable for isolated proximal muscle weakness 3/5, normal reflexes and sensation. The weakness was associated with dysarthria, aspiration, and blurry vision without diplopia. Laboratory studies were notable for BUN 37 mg/dL, Cr 2.96 mg/dL, Calcium 14.0 mg/dL, ionized calcium 7.19 mg/dL, PTH 7 pg/mL. Rheumatologic evaluation was notable for: positive ANA, dsDNA, ENA, and ANCA. PTHrP and Vit D-25 were low, and Vit D 1-25 elevated. Repeat SPEP showed a decrease in gamma globulin level and repeat skeletal survey was negative. A myomarker panel was negative. Chest CT scan showed perilymphatic ground-glass nodules with mediastinal, periportal and gastrohepatic lymphadenopathy. Bronchoscopy with biopsy of the lung nodules revealed non-caseating granulomas, negative for infectious etiologies. He was started on Prednisone 40 mg. His hypercalcemia was managed with IV hydration and calcitonin. Bisphosphonates were contraindicated given the CrCl. Brain MRI showed diffuse pachymeningeal enhancement and LP showed elevated protein concerning for Neurosarcoidosis. Dural biopsy demonstrated a single minute focus of lymphocytic infiltration, inconclusive for NS. Prednisone was then increased to 80 mg.
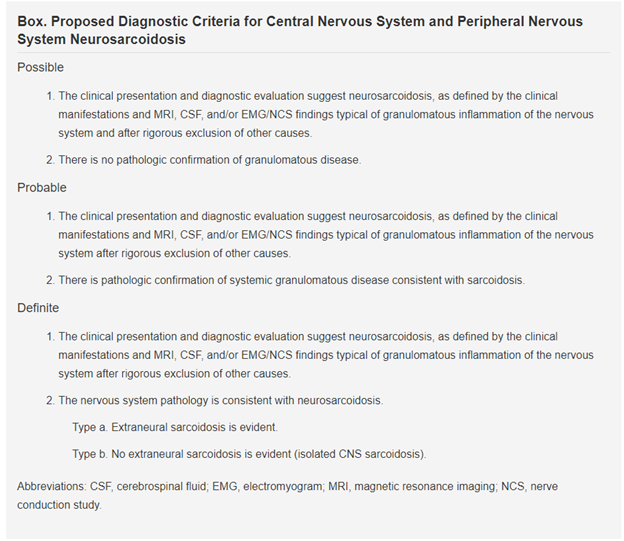
Discussion: In this report we present a patient with Probable Neurosarcoidosis who presented with chief complaint of acutely worsening lethargy with weakness and dysarthria, admitted for hypercalcemia. The differential for this patient included progression to Multiple Myeloma (MM), malignancy, primary hyperparathyroidism, and other granulomatous diseases. Given pachymeningeal enhancement, IgG4 disease was also considered. Appropriately suppressed PTH ruled out primary hyperparathyroidism. With skeletal survey negative for lytic lesions and negative bone marrow biopsy, progression from MGUS to MM was unlikely. Biopsy of lung nodules diagnosed Sarcoidosis. Brain MRI and LP findings were suggestive of a neuroinflammatory process. Dural biopsy was obtained to rule out IgG4 disease.Neurosarcoidosis is a challenging diagnosis due to diverse disease presentations and considerable variability in diagnostic definition. The Neurosarcoidosis Consortium Consensus Group panel developed a clinical definition in 2018 to encourage standardization of research that address this disease. See Figure 2. Per this definition, our patient would be classified as having Probable Neurosarcoidosis
Conclusions: Although malignancy and primary hyperparathyroidism account for almost 90% of all cases of hypercalcemia, granulomatous disorders should be considered as well. The diagnosis of NS is challenging because of overlap with other neuroinflammatory conditions and lack of systemic validation of diagnostic criteria. Per the recently created clinical definition, our patient qualifies as Probable Neurosarcoidosis. This case emphasizes the importance of a detailed clinical examination and astute diagnostic work up with critical multidisciplinary input to identify this difficult diagnosis.