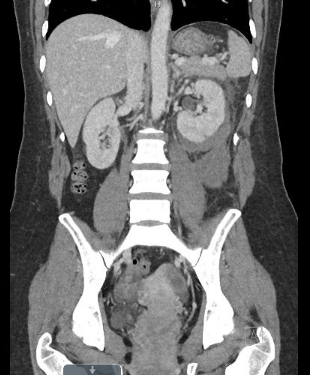
Case Presentation: A 43-year-old woman with a history of SLE underwent a renal biopsy for proteinuria without immediate complications. Four days post-procedure, she reported fever and myalgia. She was also found to have a drop in hemoglobin from 11.1 to 9.8 g/dL. A CT abdomen showed a left renal subscapular and retroperitoneal hematoma without active extravasation. Given her immunocompromised status and new fever, blood cultures were obtained and she was started on empiric antibiotics. Further workup showed elevated CRP, ESR, anti-dsDNA levels, and low complement levels. In consultation with Infectious Disease, she was trialed off antibiotics given clinical stability, lack of clear infectious source, and negative cultures. However, she continued to be febrile up to 39 C despite antipyretics and reported pleuritic chest pain. A CTA chest showed small bilateral pleural effusions. On hospital day 5, rheumatology was consulted for a possible lupus flare. Prednisone and hydroxychloroquine were added to her home mycophenolate mofetil regimen. By hospital day 7, the patient’s pleuritic chest pain and fever had resolved.
Discussion: Peri-renal hematomas occur in as many as 11% of all renal biopsies.(1) These are often self-limited and rarely require further intervention to stop the bleeding. Associated reabsorption fever is a clinical symptom that can worsen patient suffering and cause antibiotic misuse. Our case demonstrates the importance of considering non-infectious causes of fever in post-renal biopsy patients. In one large study of 2639 patients undergoing a renal biopsy, peri-renal hematoma occurred in 118 patients. Of the 57 patients with associated fever, reabsorption fever was the most common cause of post-biopsy fever, accounting for 84% of cases.(2) Only 9 cases of fever were secondary to an infection, with 3 instances due to pulmonary infection and the remainder due to secondary infection of the hematoma. The onset of reabsorption fever most commonly occurred within 4-6 days post-procedure and generally lasted one week. In our case, the patient had a non-infectious fever. It became difficult to distinguish whether her fever was due to reabsorption of the hematoma or an SLE flare. Elevated anti-dsDNA and low complement levels, pleuritic chest pain and pleural effusions made the diagnosis of an SLE flare seem more likely. SLE patients have been known to have a higher risk of complications of renal biopsy.(3) However, renal biopsy-associated SLE flare has not been documented in the literature, and is an area that would benefit from further study.
Conclusions: Reabsorption fever is the most common cause of persistent fever in post-renal biopsy patients who develop a peri-renal hematoma. These patients can be treated supportively with close monitoring without using empiric antibiotics in the absence of other clinical features of an acute infection or exacerbation of an underlying illness.