Background: On inpatient general medicine units, the timing of routine lab draws is not evidence-based, and common practice is for routine labs to be collected in the early morning. However, this collection time may not be optimal for patient satisfaction, nursing and physician workflow, and the overall efficiency of care. It is known that early morning lab draws contribute to poor sleep in hospitalized patients.(1,2) Additionally, lab results often return after a team has completed pre-rounding, which can result in delays in clinical decision-making and discharges.
Purpose: The purpose of this project was to improve patient satisfaction, increase housestaff engagement from the covering night team, and create a more balanced night nursing workflow by changing the standard lab collection time from morning to evening.
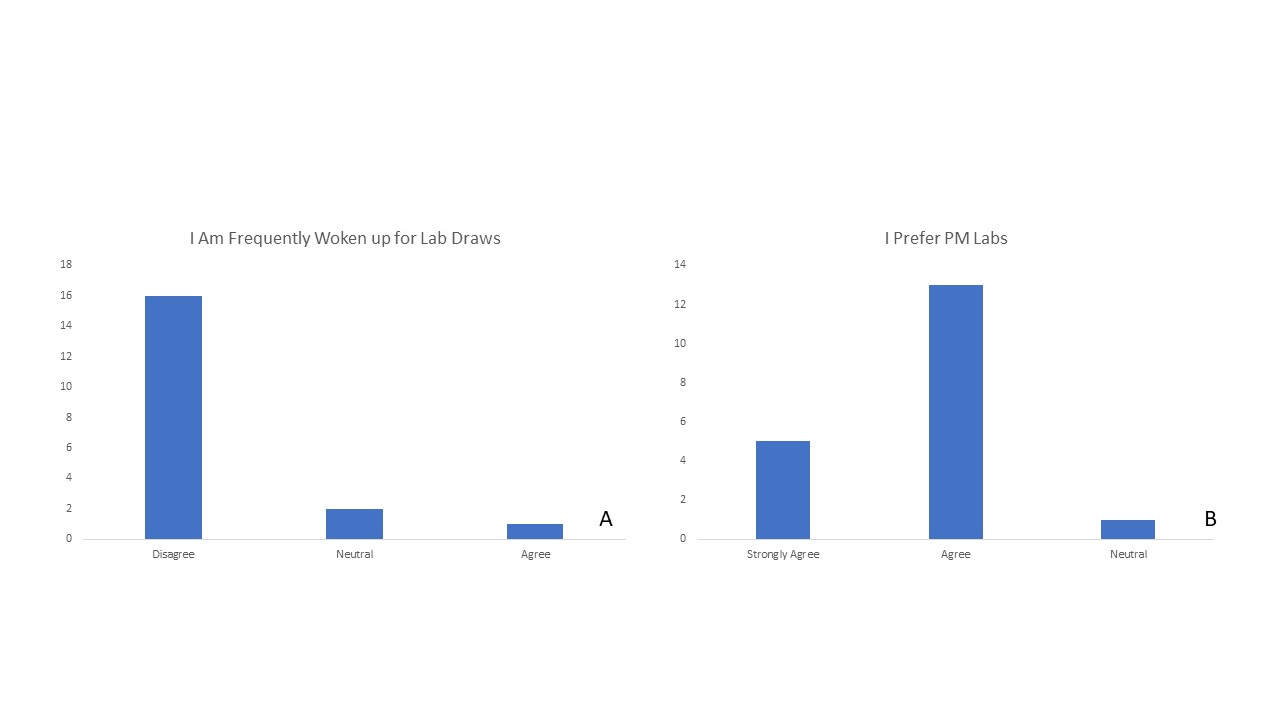
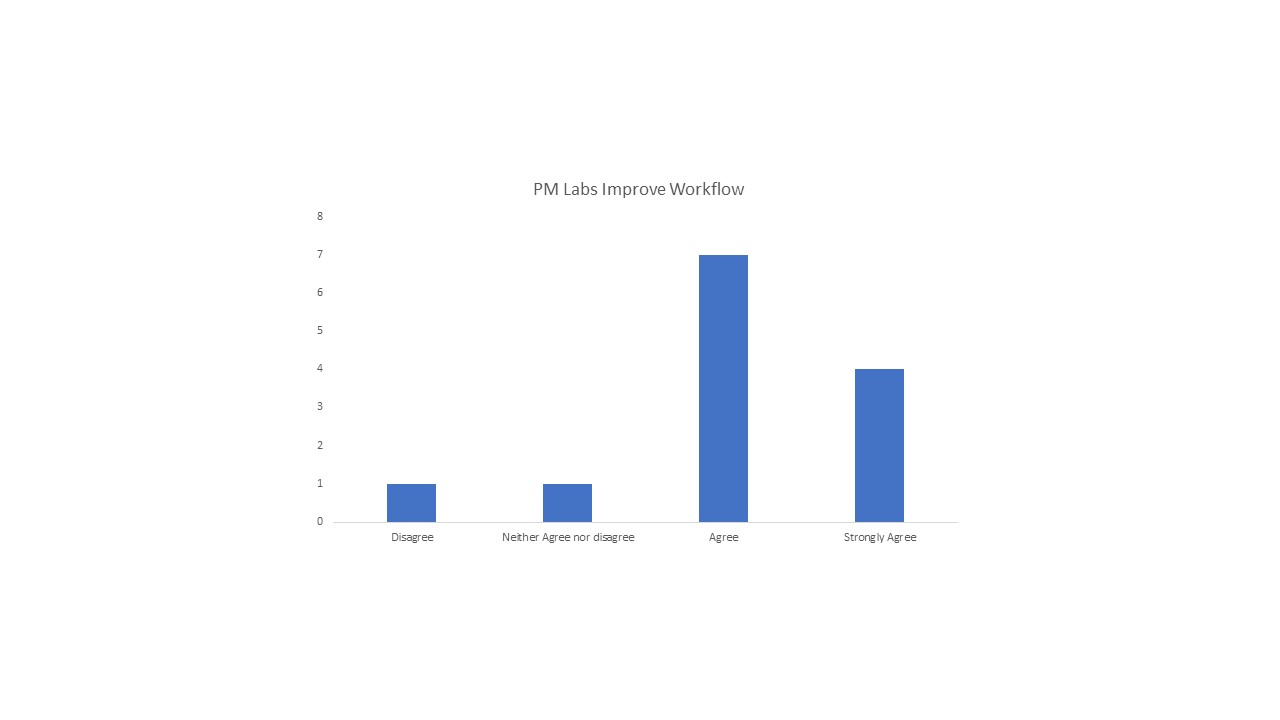
Description: Our intervention consisted of a change to the standard lab collection time from early morning (3-5 AM) to evening (8-10 PM). The general medicine unit is a 32-bed inpatient unit with two housestaff teams, each on a day and night shift schedule. Labs were still collected by the night nursing team and could be ordered by the provider more frequently than daily if clinically indicated. The night housestaff teams were responsible for reviewing lab results overnight and creating new management plans if needed. The nocturnists provided additional supervision for clinical and laboratory decompensation. The effects on patient satisfaction, nursing workflow, and housestaff engagement were evaluated through voluntary and anonymous surveys. A total of 19 patients, 16 housestaff and 13 nurses were surveyed from September to November of 2020. Additionally, the changes in laboratory turnaround time and operational metrics, including the percentage of discharge orders placed before 10 AM, were evaluated.Evening labs were favorable among patients, with 18 of 19 (94.7%) patients surveyed either agreeing or strongly agreeing that evening lab draws were preferable to morning lab draws. Only 5.3% of patients agreed that they were woken up for lab draws. Of the 13 nurses surveyed, 11 (84.6%) agreed or strongly agreed that evening labs improved their overall workflow. The reaction among housestaff was mixed, with only 33% agreeing or strongly agreeing that evening labs were preferable. While some housestaff appreciated the increased engagement provided by evening labs, others expressed concerns that there were inadequate contingency plans to address lab abnormalities that resulted overnight. From the month of August to September, the average turnaround time of a complete blood count was 38% faster and turnaround time of a basic metabolic panel was unchanged. There was no significant change in the percentage of discharge orders placed before 10 AM from August to November.
Conclusions: Evening labs are a feasible alternative to morning labs and offer a relatively easy intervention to improve patient satisfaction and nursing workflow. More work on understanding the impact on trainee education around autonomy and clinical decision-making will need to be explored. Additional work will also need to address the challenges encountered during this initial pilot program, including developing a protocol with pharmacy for warfarin dosing based on evening INR levels, as well as, adjusting anesthesia’s protocol for same day pre-procedural labs. If widely accepted, entire sections of the hospital could be divided into AM or PM lab units in order to most efficiently utilize lab resources.