Background: When COVID-19 first appeared in the U.S., few imagined the impact it would have on wellness and resilience of healthcare workers. The stress and uncertainty created by the pandemic increased secondary traumatic stress and burnout among individuals and the organization as a whole. The University of Chicago Section of Hospital Medicine came together to assess and respond to areas of need, identify opportunities for support, and shape an enduring wellness culture.
Purpose: Build a culture of wellness by responding to identified provider needs, burnout and secondary traumatic stress through the implementation of resilience-building initiatives spearheaded by a newly developed workgroup.
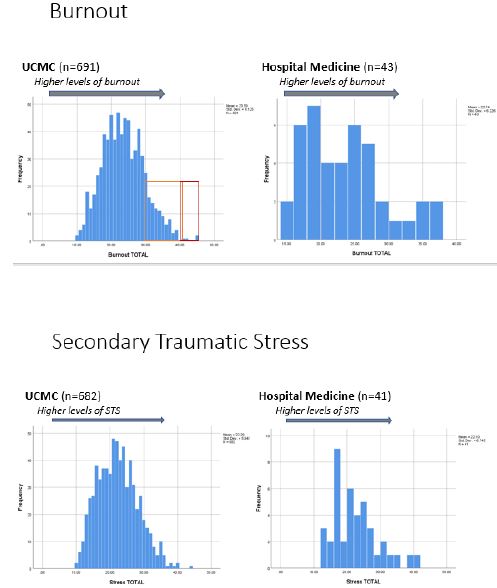
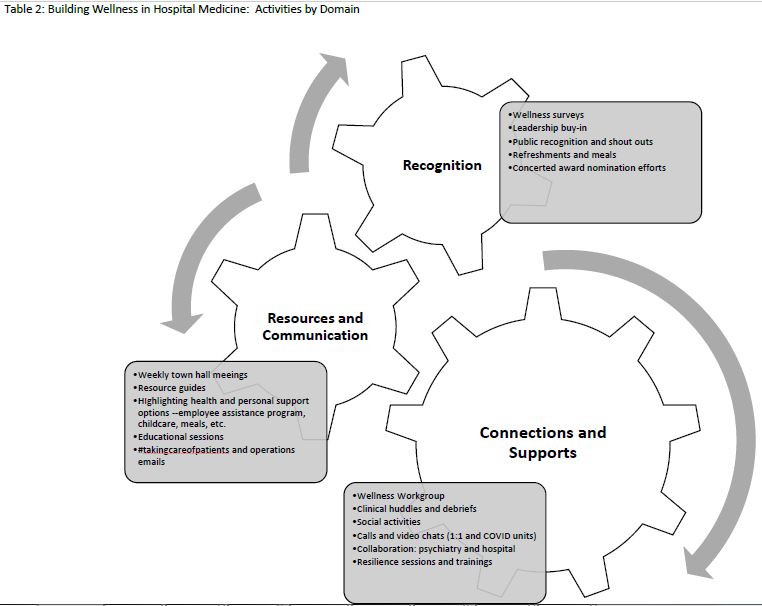
Description: After experiencing initial COVID-19 patient surges and the resultant impact, section members came together to form a wellness workgroup to identify and address the wellness needs of the group. The Section of Hospital Medicine is comprised of over 70 faculty and advanced practice providers at an 811-bed academic, urban, quaternary referral center. The challenges were multi-faceted: in addition to the need for clarity and clinical education surrounding care of COVID patients, PPE use, and rapidly shifting guidance and policies, there were also emerging needs faced by section members relating to stay at home requirements, civil unrest, family stressors, social isolation, and overall uncertainty and concern for the future. The workgroup partnered with colleagues in the department of psychiatry, who were already engaged in several institutional initiatives; specifically, administering the Professional Quality of Life (PRoQOL) scale, which examines burnout, traumatic stress, and compassion satisfaction among employees, and providing resilience skill-building trainings. Initial review of the ProQOL data from Spring 2020 comparing Hospital Medicine to the broader institution shows comparable rates of burnout and traumatic stress (Table 1). Variations in levels of compassion satisfaction and burnout were also nominally better in clinical providers, which suggests that there may be an unexplored protective element to clinical practice. As data collection is ongoing, we expect to have more nuanced comparison data to examine differences between groups and change over time by early 2021.The workgroup initiated a number of activities and practices to respond to personal and professional needs identified by section members. Three main domains emerged: 1) connections and support, 2) resources and communications, and 3) recognition (Table 2). In November 2020, section members completed a survey regarding the workgroup activities and areas of need and opportunity. Most favored activities included educational and operational updates, and COVID provider check-ins and refreshment deliveries. Qualitative data highlighted future opportunities to build resilience including: 1) reducing unnecessary work burdens, 2) support for work-life balance, 3) development of formal and informal mentorship pathways.
Conclusions: The COVID-19 pandemic led to an increase in burnout and traumatic stress among hospital medicine team members, but the opportunities for collaboration and resilience-building were also pronounced. The challenges faced offered an opportunity to better engage section members and develop and articulate a long-term vision for a “well culture” with a focus on both individual and organizational wellness.