Background: Following a hospitalization, older adults, their caregivers, and clinicians caring for them face a complex decision regarding post-acute care (PAC). The purpose of PAC, delivered by a skilled nursing facility (SNF) or home health (HH), is to support the recovery of patients after hospital discharge. However, the transition to PAC is a vulnerable time in the life of older adults, often leading to hospital readmissions and premature long-term institutionalized care. Ideally, older adults would receive the right intensity of PAC from the provider that can best meet their needs. Improved tools to standardize and facilitate choice of PAC could improve outcomes and lower costs. However, it is unknown what tools exist to help with PAC decision-making. This systematic scoping review aimed to understand the format, content, uptake, and relevant outcomes of published tools to improve patient, caregiver, and/or clinician decision making about PAC.
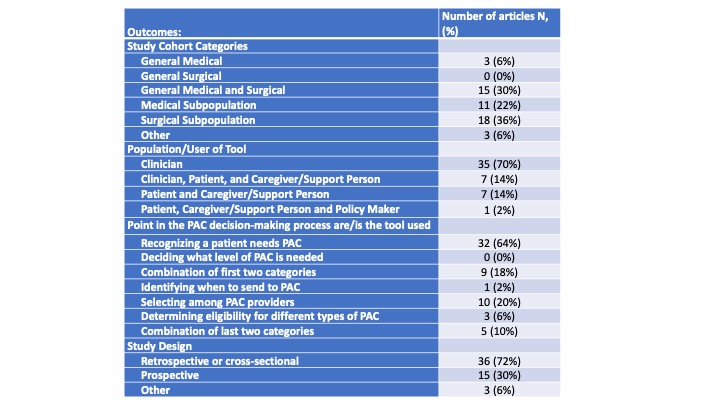
Methods: We conducted a systematic scoping review from January 1, 2011 to December 31, 2021 in PubMed and CINAHL with key words: tool, post-acute care, skilled nursing facility, home health, and hospital. We included adult community dwelling patients considering post-acute care after a hospitalization, or hospital-based clinicians who care for these patients. Articles were assessed independently, and disagreements resolved by consensus. We categorized the intended user of tool: (1) caregiver; (2) clinician; (3) policymaker; (4) patient. We also categorized the point in the PAC decision-making process where the tool is used: (1) recognizing need for PAC; (2) deciding level of PAC needed, (3) identifying when to send to PAC; (4) determining eligibility for specific PAC types; (5) presenting PAC options to choose from. We identified which types of patients were included: (1) general medicine inpatients; (2) general surgical inpatients; (3) a mix of medicine and surgery patients; (4) a specific medical subpopulation, and (5) a specific surgical subpopulation. Finally, we categorized the type of study (study design).
Results: Fifty studies met inclusion criteria. Clinicians were the most frequent intended user of the tools (n=35, 70%, Table 1). Recognizing the need for PAC was the most frequent point in the decision-making process that a tool was used (n=32, 64%). Nineteen different tools were mentioned in these 32 articles, and the most frequently mentioned were the Activity Measure for Post-Acute Care (AMPAC), Early Screen for Discharge Planning (ESDP), and Discharge Decision Support System (D2S2, n=6,3,3 respectively). Tools were most frequently developed for use in surgical subpopulations (n=18, 36%). Only 15 studies (30%) included an intervention, and of these, only 2 (4%) were randomized.
Conclusions: Surprisingly, most published tools seek to help clinicians identify patients in need of PAC and consist of prediction models derived in surgical subpopulations. Very few are patient-facing or have been tested prospectively. This suggests several important gaps that must be addressed to improve PAC decision-making. These include developing effective patient and caregiver-facing tools, broadening the populations of patients to which tools apply, testing tools prospectively to measure their feasibility, usability, and effectiveness, and broadening the types of decisions tools can help with. For example, many patients may need assistance choosing a PAC provider, or choosing among PAC options (HH vs. SNF) but very few tools have been developed for this purpose.