Background: A patient’s inpatient experience often correlates with patient satisfaction scores. These scores are measured via the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey, which collects data on patient satisfaction and perception of their hospital experience using three questions.As a tertiary academic care center, we have seen a decline in the “Medicine Division Doctor Communication” domain score since March 2020. It is probable that the COVID-19 pandemic and subsequent variant surges have limited the way physicians are able to interact with patients. Increased inpatient volume, a strict visitation policy, and COVID-19 related physician burn-out also likely contributed to making patients feel as though they were being listened to less.Our academic hospitalist group consists of fifty physicians that are responsible for seeing the majority of admitted medicine patients. Given the large size of our group, there is inevitable variation in the way that individual doctors communicate with their patients. This variability may also lend itself to differences in the inpatient experience and correlate with patient satisfaction scores.
Purpose: To improve the overall patient experience in the hospital setting by focusing on doctor-patient connection and communication.
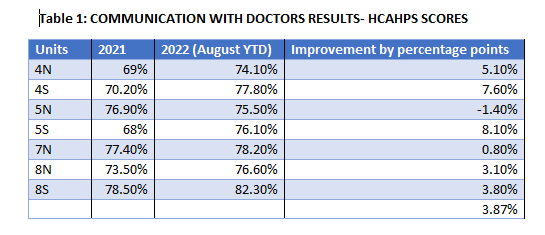
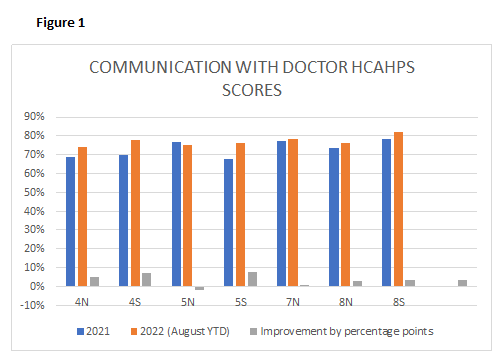
Description: Northwell Health partnered with the Clinician Experience Project, an app-based physician coaching program that consists of pre-recorded videos, reflective questions, and action plans focused on different skills, condensed into two-to-three-minute videos. Two physician-leads introduced this program at our monthly academic conferences in April 2021.The leads played the videos for the group, pausing at key moments for feedback and to reflect on real-life patient encounters. The debrief sessions also included ways to implement the tips during our daily patient encounters and discuss on how the previous sessions’ tips were employed.Hospitalists can claim credit for watching the videos, which counts towards Continuing Medical Education (CME) credits. This further incentivized our colleagues to partake in the initiative.We compared HCAHPS scores from 2021 to 2022 on non-teaching units run by our hospitalists (intervention group), as noted in Table 1 and Figure 1. We saw an overall improvement, with an average increase of 3.87% in the “Medicine Division Doctor Communication” domain score after the intervention.
Conclusions: Improving the patient experience has become a major focus of our hospitalist division, as poor scores on the HCAHPS survey can have serious financial consequences to the hospital and its employees.By viewing these short clips together about difficult scenarios and patient interactions, followed by a reflective discussion, we have managed to expand our toolbox to find solutions in dealing with patient communication. In the long term, the hope is to also create a more standard way of communicating important information to patients and promote a compassionate approach in how our core group of hospitalists interact with patients. In doing this, we aim to improve our own clinician satisfaction as we create a better connection with our patients.