Background: Mass General Brigham’s Faulkner hospital (BWFH) is a 171 bed community hospital closely affiliated with Brigham and Women’s hospital (BWH), which is located 2.5 miles away. Patient care at BWFH is supported by robust access to consultation and advanced testing from subspecialists located at BWH. To access some advanced diagnostic testing and procedures, patients are physically transported to the BWH campus, and then return to BWFH via a process called a Leave of Absence “LOA”. On average LOA is used for 1-2 patients daily. While LOA has provided access to timely tertiary care for BWFH based patients, multiple stakeholders have identified patient safety issues related to this process
Purpose: # To evaluate the current process for LOA from BWFH to BWH. # To identify best practices and opportunities for quality and safety improvement for LOA# To implement an improved process for LOA, without reducing patient access to timely advanced diagnostic or therapeutic procedures at BWH
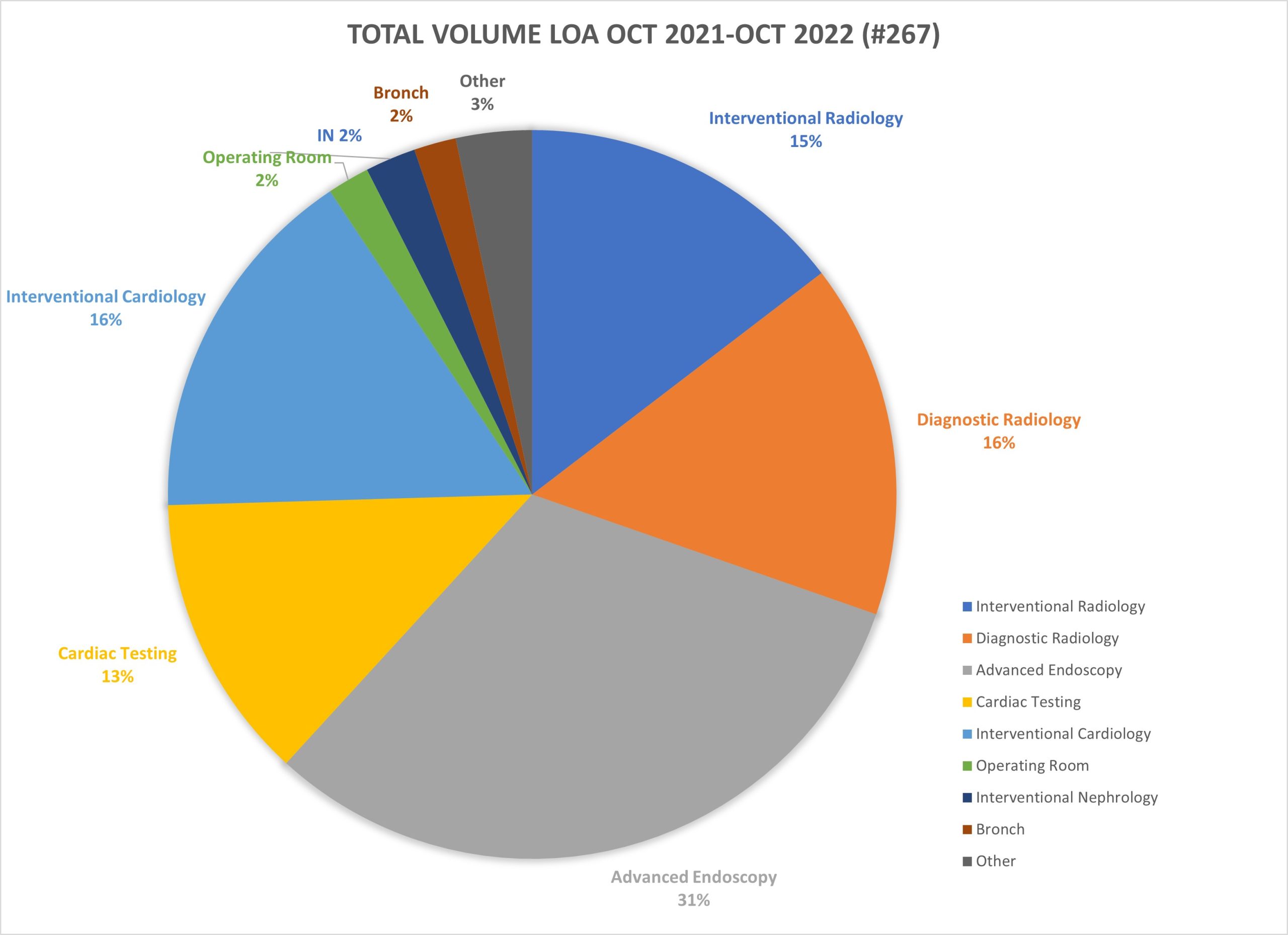
Description: The authors reviewed reports of patient safety events from a variety of sources including: formal patient safety repots, adverse event reports, patient and family relations, and individual interviews with medical providers. Qualitative interviews were conducted with all departments at both hospitals involved in the LOA process including: interventional radiology, diagnostic imaging, interventional-cardiology, gastroenterology, and cardiac testing. The authors also reviewed the volume of LOA by BWH destination department and specific test or procedure high performing departments were identified during these interviews as well as common themes for patient risk. Areas of risk included: communication and coordination of care challenges, lack of access to nursing support, no designated on campus assigned clinician, inability to dispense necessary medications including insulin or pain medications, and delayed patient transport back to the BWFH campus. Best practices models were derived from high functioning departments with enhancements built to address specific patient safety concerns. Multidisciplinary teams were invited from both BWFH and BWH campus to review these results and create engagement from stakeholders at both campuses. This resulted in a shared investment to improve work flow, and resulted in the creation of: a pre-LOA screening check list to identify high risk patients, a protocol for nursing and provider support for patients identified during screening, a new electronic medical record “EMR” based access to department specific algorithms for LOA protocols, and accurate contact information for key department personnel.
Conclusions: Access to advanced diagnostics and therapeutics via an LOA can be a valuable element of effective care in a community hospital setting. However, LOA can also present important patient safety challenges including anticipating patient risks while off campus, and coordinating the safe transition of care. Use of a pre-screening checklist can identify high risk patients and allow pre-planning for appropriate nursing support. Easy access to department specific transfer algorithms and contact information for LOA within the hospital EMR can provide effective guidance and improve communication and coordination of care. Together these interventions improve safe access to LOA, a valuable resource for timely and appropriate patient care.