Background: Compared to ten other high-income countries in the Organization for Economic Cooperation and Development (OECD), the US spent nearly twice as much on healthcare. Yet, compared to these countries, the US has the lowest life expectancy. This disparity will worsen as the US’s national healthcare expenditures rise from $4.1 trillion in 2020 to a projected $6.2 trillion in 2028.Over 7 billion labs tests are performed annually in the US. Diagnostic laboratory tests comprise a significant component of these high healthcare expenditures. Yet, depending on the strictness of criteria applied, anywhere from 8% to 30% of diagnostics were redundant. In fact, as patients are passed from one provider to the next, laboratory testing is often times repeated, needlessly adding to total healthcare costs and also subjecting the patient to discomfort. Repeat tests at one particular lab accounted for 17% of all lab orders and an estimated $130,000 in unnecessary expenses.
Purpose: Against this backdrop, both the Society of Hospital Medicine (as part of the Choosing Wisely) and the Critical Care Society collaborative have made the avoidance of repetitive lab testing a top recommendation. Looking towards Complete Blood Counts (CBCs), Feldhammer et al illustrate the redundancy of lab tests, highlighting that nearly 55% of CBCs are ordered within 23 hours of a prior CBC.While some methodologies work well in a single unit, they face challenges in terms of scaling to multiple units within a hospital and scaling to multiple hospitals. Further, they struggle to account for both housestaff and attending turnover.
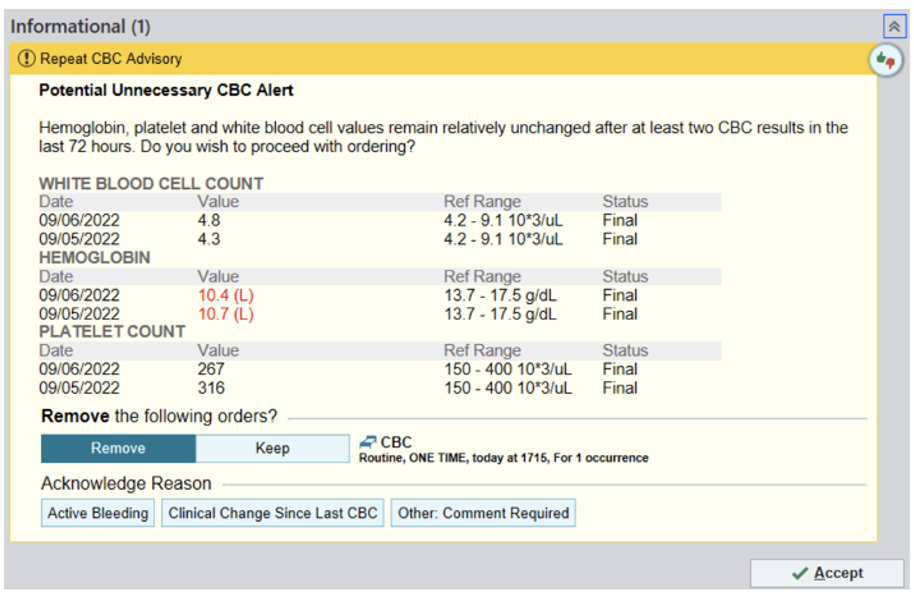
Description: At New York University (NYU), we implemented a Best Practice Advisory (BPA) in Epic, our EMR used across 4 hospitals (NYU Langone – 674 beds, NYU Orthopedic – 225 beds, NYU Brooklyn – 450 beds, NYU Long Island – 591 beds) in our system. The objective of our study was to examine whether a BPA could nudge providers towards ordering less unnecessary CBCs (without reducing the quality of clinical care) and to understand what amount of cost could be saved by doing so.Via a multidisciplinary team, we designed the BPA (Figure 1) and defined the term “potentially unnecessary” with respect to CBCs. A CBC was considered potentially unnecessary if the two most recent CBCs within the last 72-hour window had all the following: a White Blood Cell (WBC) count between 4,000 to 12,000/µL, a Hemoglobin (Hgb) >8 g/dL, a Hgb change < 1 g/dL, and a platelet count between 150,000 – 400,000/µL.
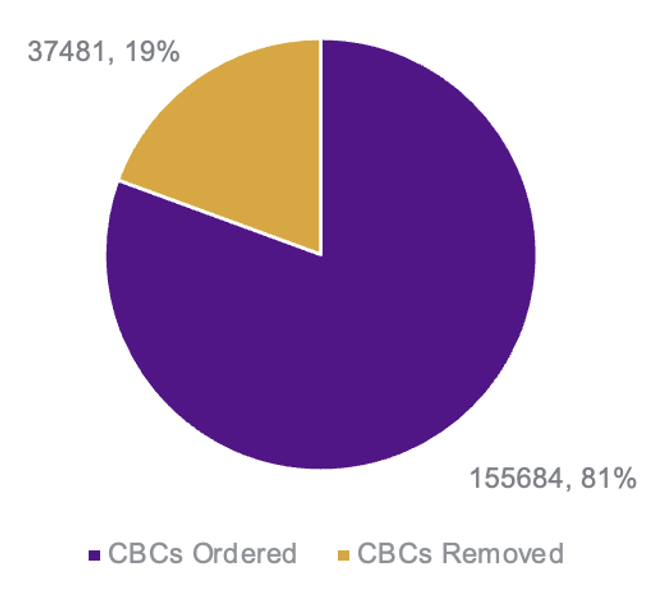
Conclusions: Over 2.5 years, we measured BPA success where success was achieved if the end-user did not order a CBC within two hours of the BPA firing. Of the 193,000 times the BPA fired over a 28-month period, end-users did not order a CBC nearly 37,000 times, resulting in a 20% reduction in the number of CBCs ordered (Figure 2). Furthermore, if we consider the approximate cost of the CBC reagent to be $10 (based on internal metrics), this translates to a cost reduction of $375,000. In addition, if we use an external metric such as Quest, the approximate cost of a CBC test is $29. With this approximation, the estimated cost reduction approaches $1.1 million.Our study is unique in that it implements a novel BPA based on the two most recent CBCs in a 72-hour period. In addition, given standardization in our criteria and by presenting the information to the right provider at the time of ordering, we were able to launch a successful health system wide initiative that can be replicated to facilitate reduction of other lab tests and potentially imaging tests in the future.