Background: Consumer satisfaction is largely dependent on convenience, efficiency, and quality, and healthcare is no outlier. Technological advancements, such as the use of artificial intelligence or virtual visit appointments, is emerging as a new form of healthcare provided. While these technologies have existed far before the COVID-19 pandemic, it has expedited the mass population’s acclimation to digital therapeutics within healthcare. One such technology is remote patient monitoring (RPM) which allow healthcare providers to track and follow a patient’s health status without their physical presence in a healthcare setting. RPM can be achieved through different mediums such as wearable devices, sensors, and mobile applications. RPM appears to “keep up with the times” as it allows patients to be in the comfort of their own home, provides real time feedback to providers, and improves patient health.
Purpose: Previous studies of RPM programs explore their efficacy. Studies show that RPM programs can potentially have large benefits within the healthcare ecosystem as they can lead to lower number of hospitalizations, decrease risk for readmissions, and reduce costs. However, limited research delves into the factors that affect patients’ engagement with an RPM program. Therefore, the purpose of this investigation is to assess factors that affect user engagement with the implementation of an innovative RPM program.
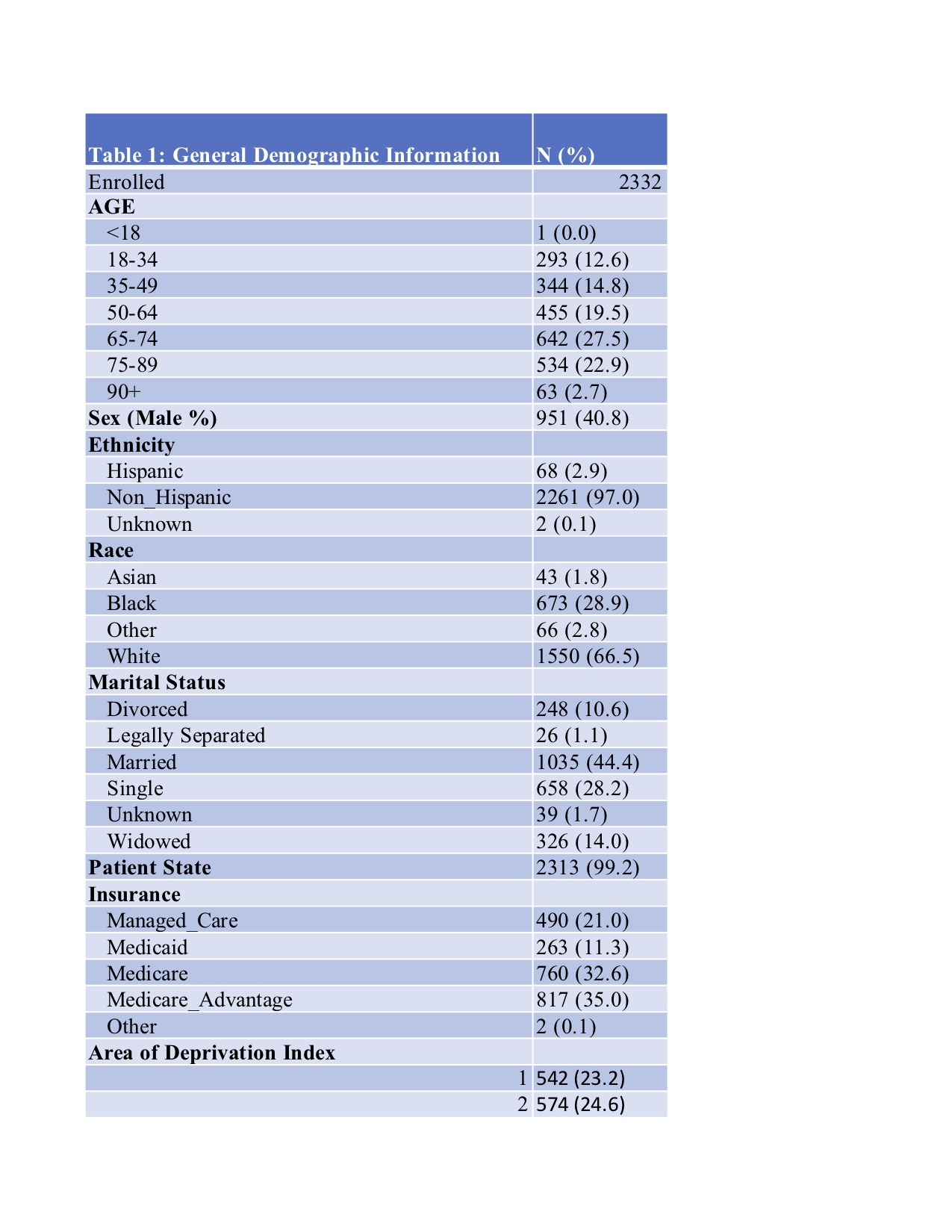
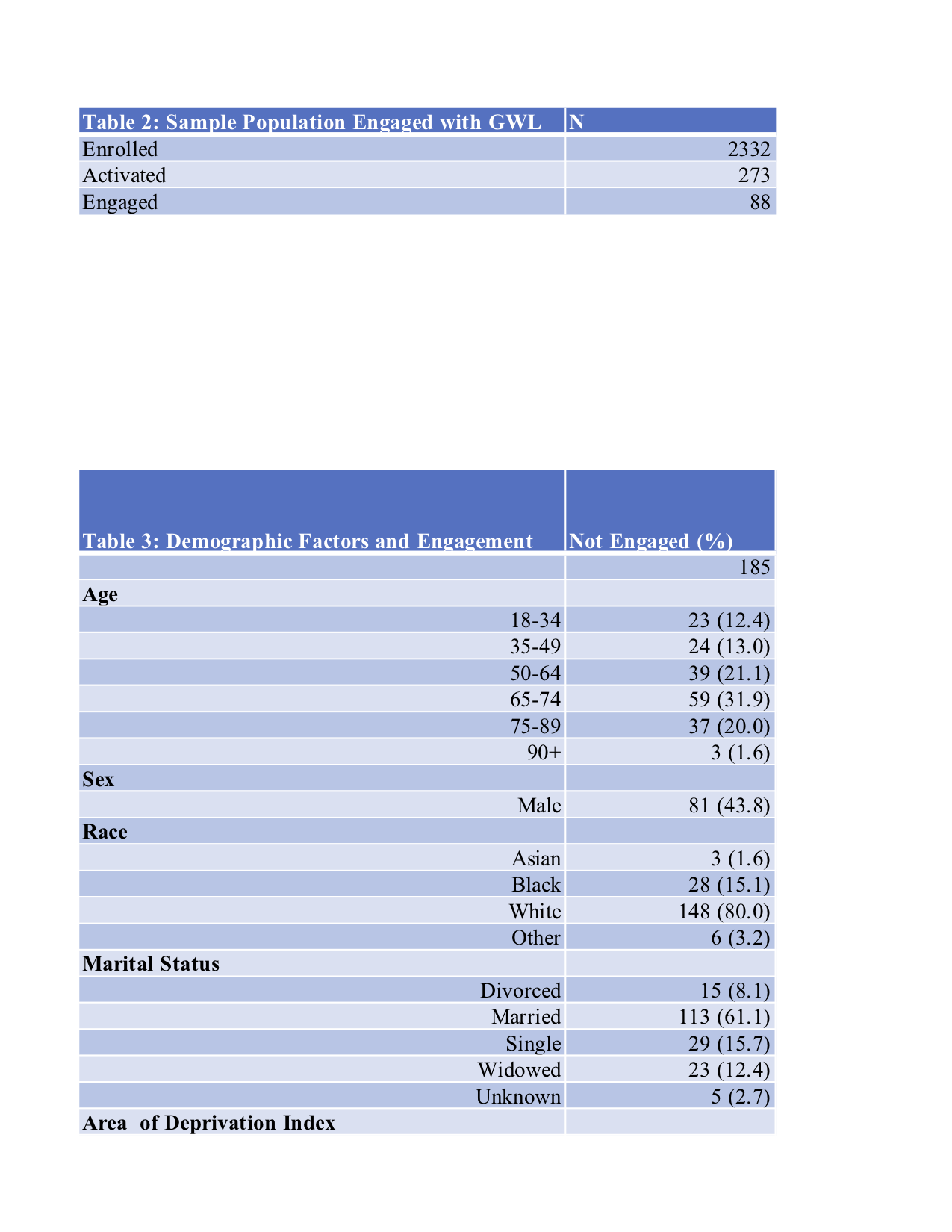
Description: GetWell Loop (GWL) is a mobile health application serving as an RPM program within the Froedtert Health system where post-discharge hospitalized patients had the option of being enrolled in the GWL service. Through this mobile app, patients were able to update their providers regarding their day-to-day health status through virtual questionnaires, submit questions, and receive feedback in real time. All inpatient hospital discharges within the Froedtert Health system between March 2020 – November 2020 were stratified on readmission risk (low, medium, high). Low-risk patients were offered access to GWL, while moderate-risk and high-risk patients were offered access to GWL and the conventional care coordination. Demographic data was obtained from EPIC, while GWL specific usage was obtained from the GWL application. Various demographic variables were being analyzed such as patient age, patient sex, marital status, and risk level for hospital readmission. Engagement was defined as an engagement score of greater than 50%. This number is a calculation of the number of touchpoints the user engaged with the application compared to the total number of touchpoints offered by the GWL application. Univariate and chi-squared analysis was used to examine demographic and user differences between users who engaged in the application and those who did not. Multivariate analysis was then run to control for all factors to determine true significance.
Conclusions: Preliminary data suggests that patients with a low risk level for readmission are approximately two times more likely to be engaged with GWL than high risk level patients. There were no significant differences in engagement between age, sex, race, language, insurance provider type, or area of deprivation indexInformation from this study can help inform health systems on how to better implement such technologies more appropriately and efficiently. Maximizing the understanding of when and where RPM programs are the most useful can help towards achieving better patient care, higher patient satisfaction, and improved outcomes.