Case Presentation: A 75-year-old male with a history of type 2 diabetes mellitus, atrial fibrillation and hypertension presents to the hospital for evaluation of generalized weakness. He was found to have significant anemia with hemoglobin of 6.5 g/dL. He has had multiple admissions for anemia, and in the last year has required over twenty blood transfusions. Anemic workup was initiated including a complete blood count showing normocytic anemia with a markedly reduced reticulocyte count of < 0.5%. Further workup including iron studies, folic acid, vitamin B12, LDH, haptoglobin, Direct and Indirect Coombs testing, and fecal occult blood testing were all unremarkable except for elevated transferrin. He was evaluated for underlying infection and all viral and bacterial workup including parvovirus B19, HIV, EBV, CMV, babesiosis, and other tick-borne illnesses were negative. He was evaluated for plasma cell disorders and quantitative immunoglobulins, free light chains with serum electrophoresis and immunofixation, and peripheral smear were also all unremarkable. The patient underwent invasive investigation by means of commuted tomography angiography of the chest, abdomen, and pelvis, upper and lower endoscopies, and a bone marrow (BM) biopsy which continued to be unrevealing in the cause of his anemia. Further laboratory studies were obtained, and he was noted to have elevated inflammatory enzymes and a significantly elevated antinuclear antibody titer of 1:1280. Further autoimmune workup was unremarkable. He was started on hydroxychloroquine by rheumatology, but his anemia persisted. He was referred for a repeat bone marrow biopsy which was diagnostic for pure red cell aplasia (PRCA). Hydroxychloroquine was promptly discontinued, and cyclosporine 200 mg twice daily and weekly intravenous dexamethasone was initiated. Over the next few months, his cyclosporine was reduced to 50 mg twice daily and his dexamethasone tapered off without any need for repeat blood transfusions. With time, the hemoglobin normalized, and his symptoms were greatly improved.
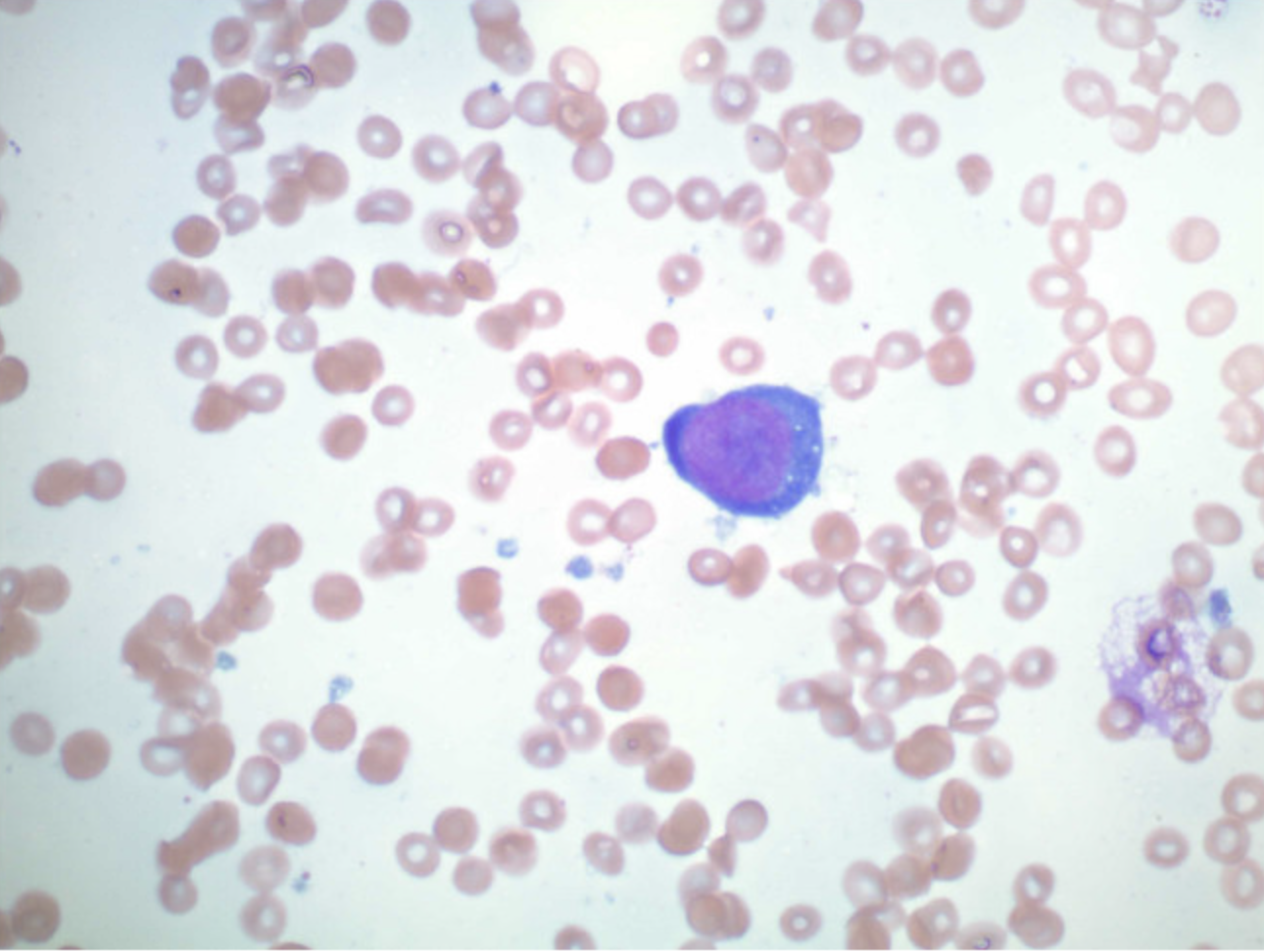
Discussion: PRCA is a rare form of bone marrow suppression where autoantibodies are formed against red blood cell (RBC) precursors or erythropoietin, which then interfere with RBC production. It can be associated with various diseases, including myeloproliferative and lymphoproliferative disorders, autoimmune diseases, thymoma, medications, and infections. PRCA is a rare hematologic disorder that occurs equally in males and females. It should be considered in the differential in patients with isolated anemia and reticulocytopenia in the presence of normal platelet and white cell count. A BM biopsy that shows an absence or reduced number of erythroblasts is diagnostic. However, in this case, the patient needed a second BM biopsy to prove he had PRCA. The therapeutic management of PRCA is with immunosuppression. This is achieved by cyclosporine, a potent immunomodulatory agent that inhibits the production of cytokines involved in regulation of T-cell activation. Cyclosporine A may be used with or without corticosteroids.
Conclusions: This was a case of an acquired PRCA in an elderly male who has had chronic anemia with recurrent blood transfusions for the past 20 years. It is vital to know that PRCA has an incidence rate of 1.06 patients per million per year. As a result, PRCA is noted to be extremely rare and prompt treatment should be initiated to avoid further transfusions.