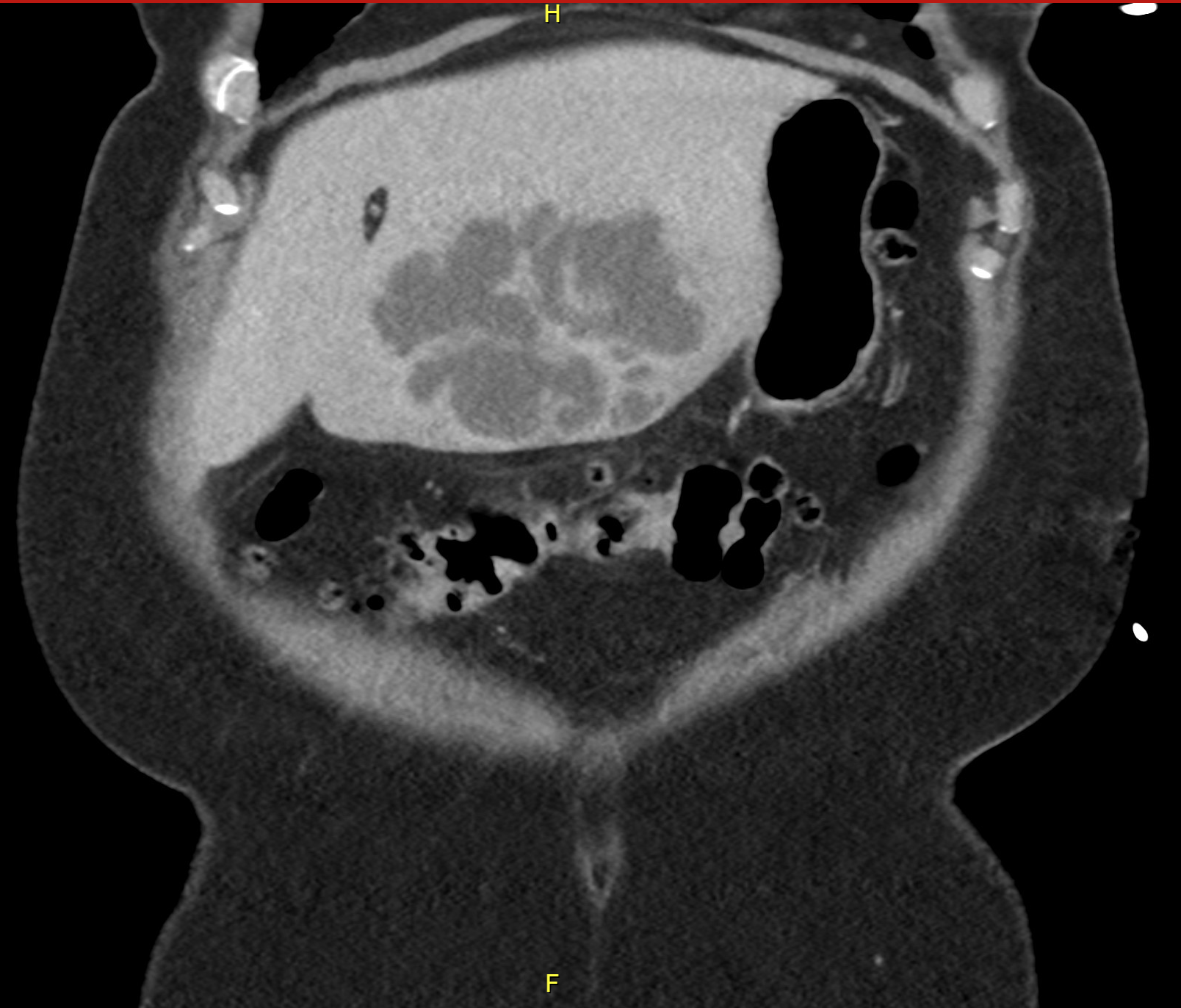
Case Presentation: A 69-year-old woman with hypertension and arthritis presented with 2 weeks of myalgias, decreased appetite, malaise, and fevers. She also reported two days of non-bloody diarrhea that had since resolved. She denied any recent travel, abdominal or dental procedures, or contact with livestock. Vital signs were notable for the absence of fever. Physical exam was unremarkable. Laboratory findings revealed elevated white blood cell count of 22×109/L and elevated transaminases (Alkaline Phosphatase = 190 IU/L, AST = 102 IU/L, ALT = 93 IU/L). Computed tomography scan of her abdomen and pelvis demonstrated a left hepatic multiloculated cystic lesion that measured 5.4 x 9.0 x 6.3 cm3 with peripheral enhancement concerning for a hepatic abscess. She was started on Piperacillin-Tazobactam. A pigtail catheter was placed for drainage. Cultures grew Parvimonas micra. She was transitioned to intravenous ampicillin-sulbactam for 3 weeks and subsequently placed on clindamycin for an additional 2 weeks. Complete resolution was noted on imaging at the end of therapy.
Discussion: Parvimonas micra (P. micra) is a commensal bacterium of the human oral flora and gastrointestinal tract. Infections with P. micra outside of the oral cavity are uncommon. P. micra has been implicated in abscess of the spine, chest wall, and brain, as well as meningitis, septic arthritis, spondylodiscitis, empyemas, and endocarditis. Hepatic abscess due to P. micra was first reported in a 90-year-old woman with ovarian cancer in 2018; she did not survive. Since then, there have only been a handful of cases reported; most of these occurred outside the United States. Risk factors identified in the literature include social isolation, low socioeconomic status, poor hygiene, and immunocompromise. Our patient did not have any of the aforementioned risk factors. P. micra is difficult to identify because of its lack of clinical symptoms, slow growth, and the need for special culture media and identification methods. Recent improvements in microbiology laboratory technology have likely contributed to the pathogen’s emergence in the literature.
Conclusions: We aim to highlight this rare cause of hepatic abscess to help guide future recognition and management of this condition. Untreated, hepatic abscesses are often fatal, regardless of the causative organism. Prompt empiric treatment with antibiotics and surgical drainage are recommended. Treatment of P. micra should be guided by susceptibility results; typically, P. micra is sensitive to metronidazole, clindamycin, and penicillin. Patients with good response to surgical drainage should be treated with 2-4 weeks of parenteral therapy followed by 2 weeks of oral antibiotics, while those with incomplete drainage should receive 4-6 weeks of parenteral therapy. The prognosis of hepatic abscesses due to P.micra is good and similar to other common pathogens in the absence of malignancy and adequate surgical drainage. Due to the high incidence of hepatic abscess formation in the setting of malignancy, a thorough work-up for primary cancers should be pursued.