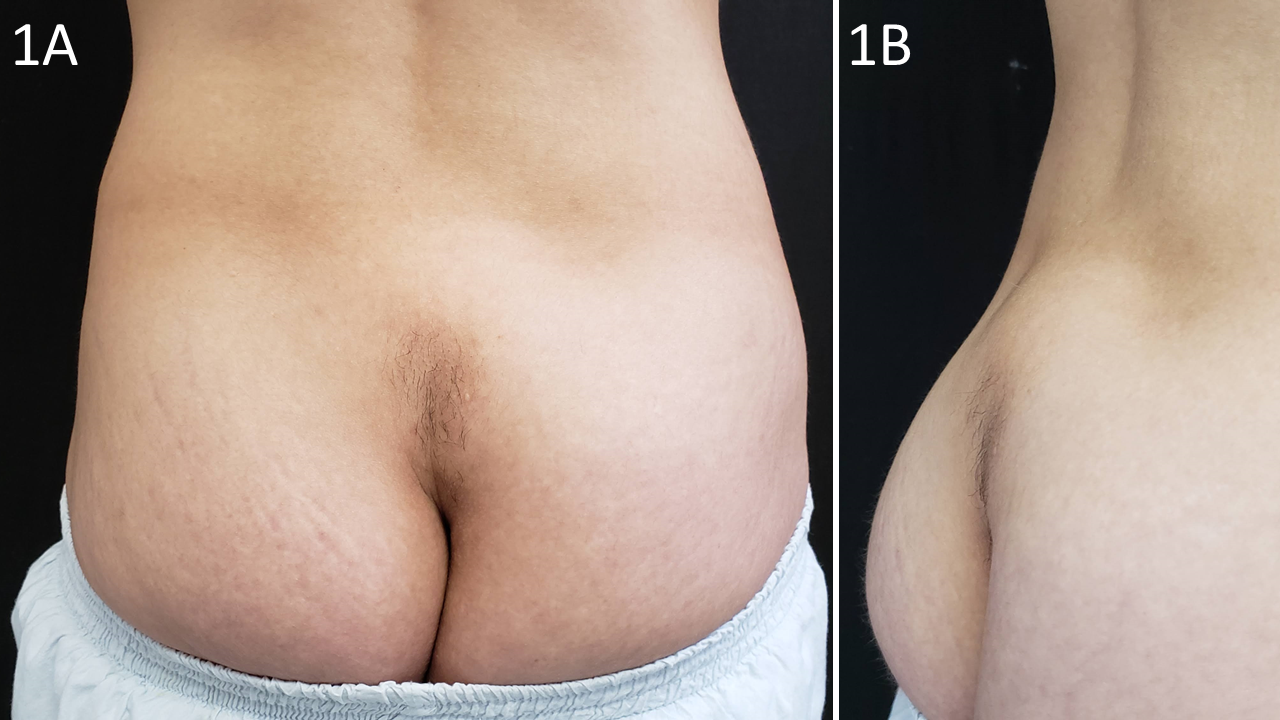
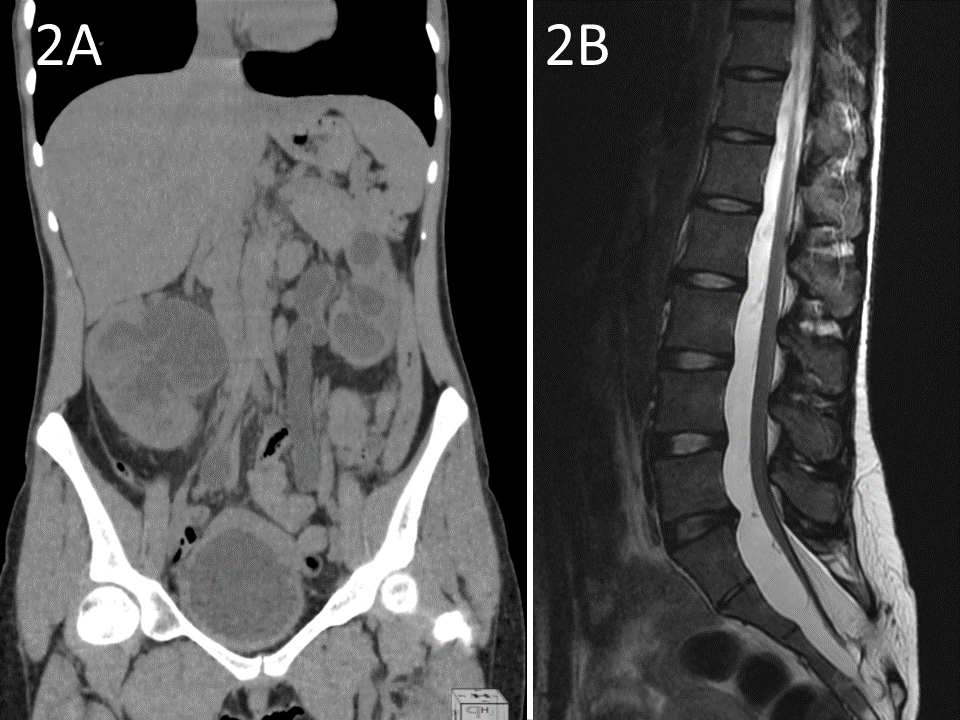
Case Presentation: We report a case of a 21-year-old woman presenting with repeated urinary tract infections, urinary incontinence, and hypertension over the course of 3 years. She denied other symptoms. She reported an uneventful C-section delivery, 3 years earlier also, of her first and only pregnancy, that coincidentally was followed by the onset of the current presentation. PMH and ROS were negative. Physical examination was pertinent for a palpable mass in the right flank and a bulging with localized hypertrichosis in the sacral region [images 1A and 1B]. Laboratory findings were significant for acute-on-chronic renal failure (CKD-EPI GFR of 11mL/min/1.73m²) and normocytic normochromic anemia. CT scan of the abdomen revealed bilateral ureterohydronephrosis and diffuse parietal bladder thickening [image 2A], as well as a lumbosacral spine defect. MRI confirmed the hypothesis of spina bifida occulta (SBO) in the sacral region and demonstrated an association with tethered cord syndrome (TCS) [image 2B]. Besides urinary symptomatology, the patient had no other signs or symptoms resulting from the evident imaging of neurological abnormality. Neurosurgery recommended conservative management of TCS. The patient was discharged after a cycle of antimicrobial therapy for UTI and partial improvement of renal function. She underwent adequate training for intermittent catheterization with follow-up for CKD and bladder dysfunction at an outpatient clinic.
Discussion: Spina bifida is a congenital malformation resulting from failed closure of the embryonic neural tube in which the spinal column is split/bifid. Vertebrae at the level of the defect lack neural arches and are incomplete dorsally. In SBO, the meninges and/or neural tissue remain underneath the skin. This defect is often suggested by a cutaneous manifestation such as a hairy patch, dimple, hemangioma, lipoma, or dermal sinus tract. It may be found in up to 10% of the population and usually occurs in the lumbar region. In SBO, the meninges or neural tissue remain covered by the skin. The term sacral spina bifida occulta (SSBO) has been used to describe defects spreading from S1-S5. Diagnosis of TCS depends mostly on the clinical scenario and radiological criteria, in which the presence of a thickened filum terminale and a low-lying conus medullaris in symptomatic patients is indicative of this condition. SBBO is usually associated with complications, such as posterior disc herniation, neurological abnormalities of the feet, enuresis, and functional disorders of the lower urinary tract. Abnormal traction on the spinal cord in TCS may result in ischemia and thus lead to motor, sensory, and urinary neurological deficits. Our patient had local skin, subcutaneous, and urinary tract abnormalities, with no other relevant findings on thorough ROS and careful physical examination.
Conclusions: This 21-year-old woman had an undiagnosed congenital abnormality in which an attentive physical examination could have raised this diagnostic hypothesis many years before the development of the described complications, particularly CKD. We postulate the onset of clinical course began at/after pregnancy due to changes in spine conformation associated with compression of intra-abdominal organs, perhaps with a potential role of an unreported C-section spinal anesthesia complication. Therefore, taking a thorough medical history with proper PE remains of the utmost importance.