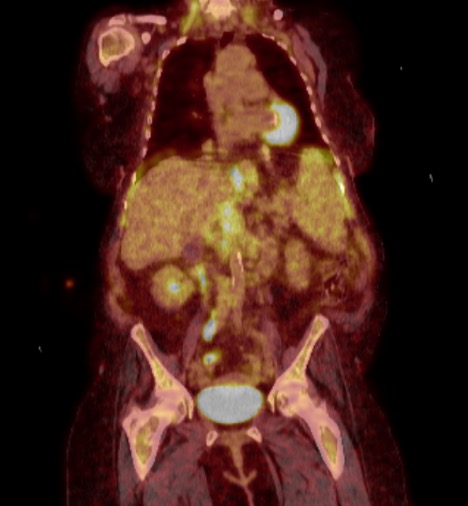
Case Presentation: An 88 year-old woman with a history of atrial fibrillation, hypertension, anemia, and mild thrombocytopenia presented to the emergency department with diarrhea, nausea, pre-syncope, and weakness. She had diarrhea for the last 1-2 years, but had worsened over the previous few weeks, with 10-12 loose stools per day. She also reported early satiety and a 20-lb weight loss over the previous 6 months. Of note, she had an eight-year history of anemia, with a normal CT abdomen/pelvis two years prior; she had declined a bone marrow biopsy or colonoscopy. On admission, her complete blood count was near baseline with WBC 6 K/uL with monocytosis (29%) and lymphopenia, Hg 9.4 g/dL and platelets 112,000 K/uL; CRP 5.5 mg/dL; and mild elevation in ALP to 241 U/L. A flexible sigmoidoscopy noted diffuse low-grade inactive chronic colitis. Biopsy showed diffuse mild plasmacytosis in the lamina propria, which could be consistent with microscopic colitis although pathology noted appearance was atypical. She was started on budesonide without improvement. Given an abnormal abdominal ultrasound, an MRCP was performed and notable for numerous abnormal lymph nodes in the retroperitoneum and mesentery suspicious for lymphoma and acquired hemosiderosis of the liver and spleen with splenomegaly. PET scan (see figure) confirmed multiple metabolically active lymph nodes consistent with lymphoma. A lymph node biopsy was unsuccessful. Ultimately, a bone marrow biopsy revealed systemic mastocytosis with an associated non-mast cell hematological neoplasm (chronic myelomonocytic leukemia). Elevated serum tryptase and KIT D816V mutation further confirmed the diagnosis. The patient was discharged on famotidine and cetirizine along with EpiPen prescription but due to ongoing gastrointestinal symptoms, was escalated to cromolyn. She ultimately required initiation of avapritinib, a tyrosine kinase inhibitor, with symptomatic improvement.
Discussion: Mast cell disorders can typically be broken down into two categories of either normal mast cell numbers with abnormal activation (secondary) or as in this case, clonal/primary where neoplastic mast cells accumulate in tissues. In both instances, symptoms are often due to mast cell release of tryptase, histamine, and other mediators producing symptoms similar to allergic reactions with specific symptoms such as rashes, GI symptoms, cytopenias, etc dependent on location of mast cell accumulation. Given the non-specific symptoms and relatively rarity of systemic mastocytosis, there is often a delay in diagnosis. The diagnosis is confirmed by WHO classification. It is most common to have skin, bone marrow, and GI tract involvement whereas liver, spleen, and lymph node involvement, as seen in this patient, is more rare. There is less data on systemic mastocytosis in those over 70 years old, but it is known that older age is predictive of poorer prognosis and associated hematologic malignancy (SM-AHN) is common. Regardless of treatment choice, response to therapy is monitored by both clinical response and reduction in mast cell infiltrates and tryptase levels.
Conclusions: Systemic mastocytosis is a rare cause of diarrhea but should be considered in any patient with concomitant cytopenias, rashes, or anaphylactic symptoms.