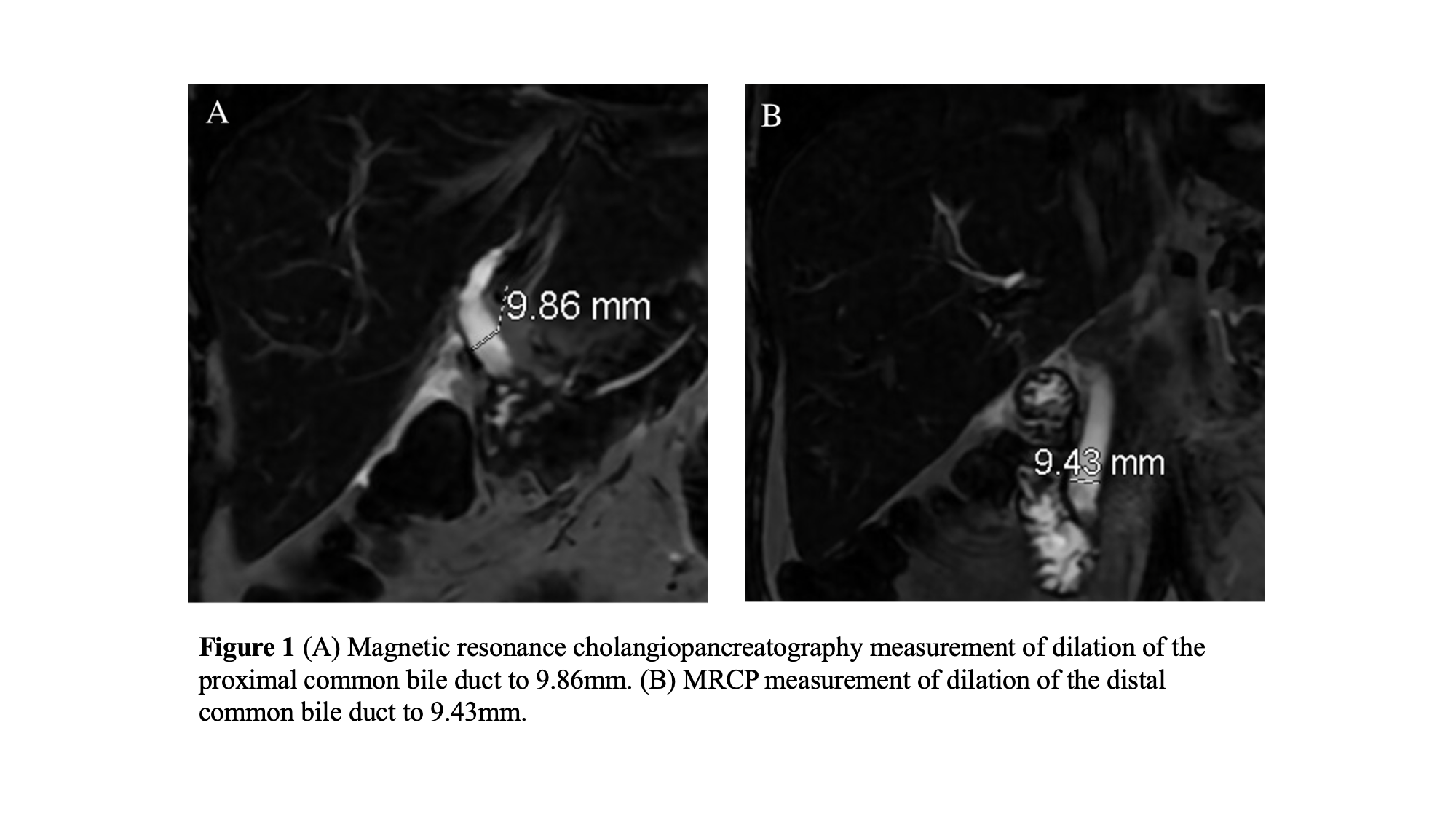
Case Presentation: A 57-year-old female with hypertension, hyperlipidemia and a surgical history of cholecystectomy for gallstone pancreatitis six years ago presents with right upper quadrant (RUQ) abdominal pain, nausea, vomiting, and skin yellowing for one day. Over the prior eight months, the patient had experienced intermittent episodes of RUQ abdominal pain that self-resolved in minutes. On the day of presentation, the patient had sharp, persistent RUQ abdominal pain and multiple episodes of non-bilious, non-bloody vomiting. Upon presentation, she was febrile to 102.5F, hypertensive to 167/77 mm Hg, with pulse 90 bpm, and O2 saturation 100%. Her exam was notable for icteric sclera, jaundice from head to abdomen, diffuse abdominal tenderness without rebound or guarding, and positive Murphy’s sign. Her liver enzymes were abnormal: ALP 434 U/L, ALT 458 U/L, AST 1455 U/L, total bilirubin 1.2 mg/dL, and direct bilirubin 0.5 mg/dL. The white blood cell count, troponin, and lipase were within normal limits. Abdominal ultrasound showed a moderately dilated common bile duct. The patient was started on piperacillin-tazobactam and admitted. The next morning, her fever, pain, nausea, and vomiting improved. New laboratory results showed elevated ALP (418 U/L), ALT (501 U/L), AST (309 U/L), total bilirubin (4.7 mg/dL) and direct bilirubin (3.2 mg/dL). MRCP revealed biliary dilation to nearly 10mm with smooth tapering to the ampulla, without obstruction (Fig. 1). The following day, the patient’s liver enzymes downtrended and her symptoms resolved. ERCP was deferred due to her clinical improvement and she was discharged on levofloxacin and metronidazole with gastroenterology follow-up.
Discussion: In this report, we present a patient with acute cholangitis following remote cholecystectomy. The diagnostic criteria for acute cholangitis includes evidence of systemic inflammation and cholestasis with imagining demonstrating biliary dilation/evidence of an underlying etiology. This patient met all but the last criteria – her MRCP revealed expected post-cholecystectomy dilation. However, imaging was not completed until after symptomatic improvement. Overall, the clinical picture is suspicious for a passed stone undetected due to delayed imaging. Post-cholecystectomy choledocholithiasis is rare, and the frequency with which it results in ascending infection is not well documented; detailed description of such instances is limited to case reports [1-3]. We present this case to add to this small collection of literature. Surgical clip migration [4-7] and biliary strictures [8] have been reported as niduses for post-cholecystectomy choledocholithiasis. Additional risk factors in a limited body of research include older age, the presence of multiple common bile duct stones upon gallbladder removal, and the presence of periampullary diverticula [9-10]. This patient did not have a clear nidus for stone formation on imaging – no migratory clips or strictures, no periampullary diverticula noted – though it is possible that these were present but not well visualized. Alternatively, she may have had a chronically retained, newly migratory stone.
Conclusions: Hospitalists commonly care for patients with cholecystitis or acute cholangitis, but it is rare that those patients have a surgically absent gallbladder. Evidence regarding risk factors for post-cholecystectomy choledocholithiasis is limited, and a clear nidus for stone formation is not universally identified.