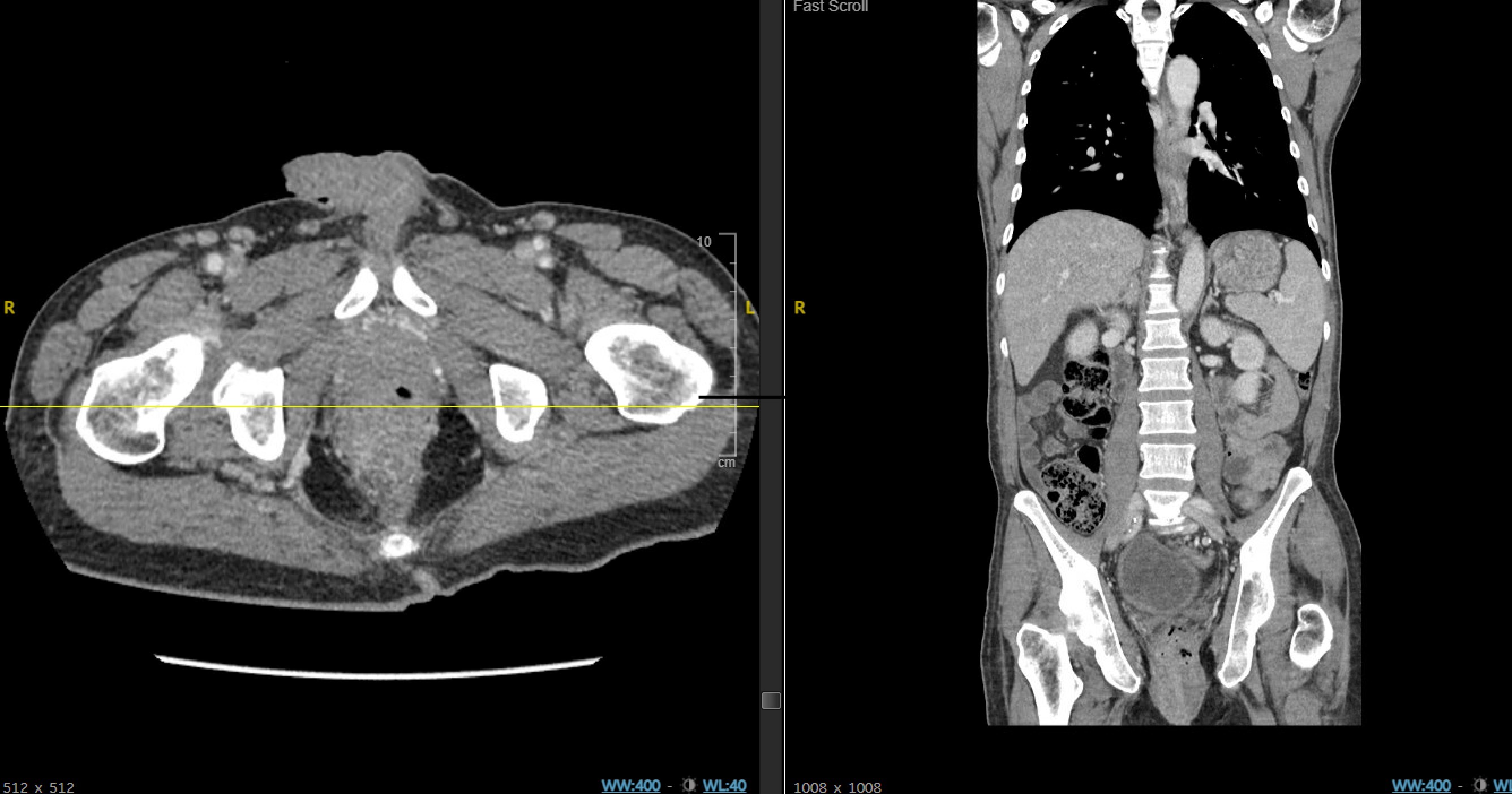
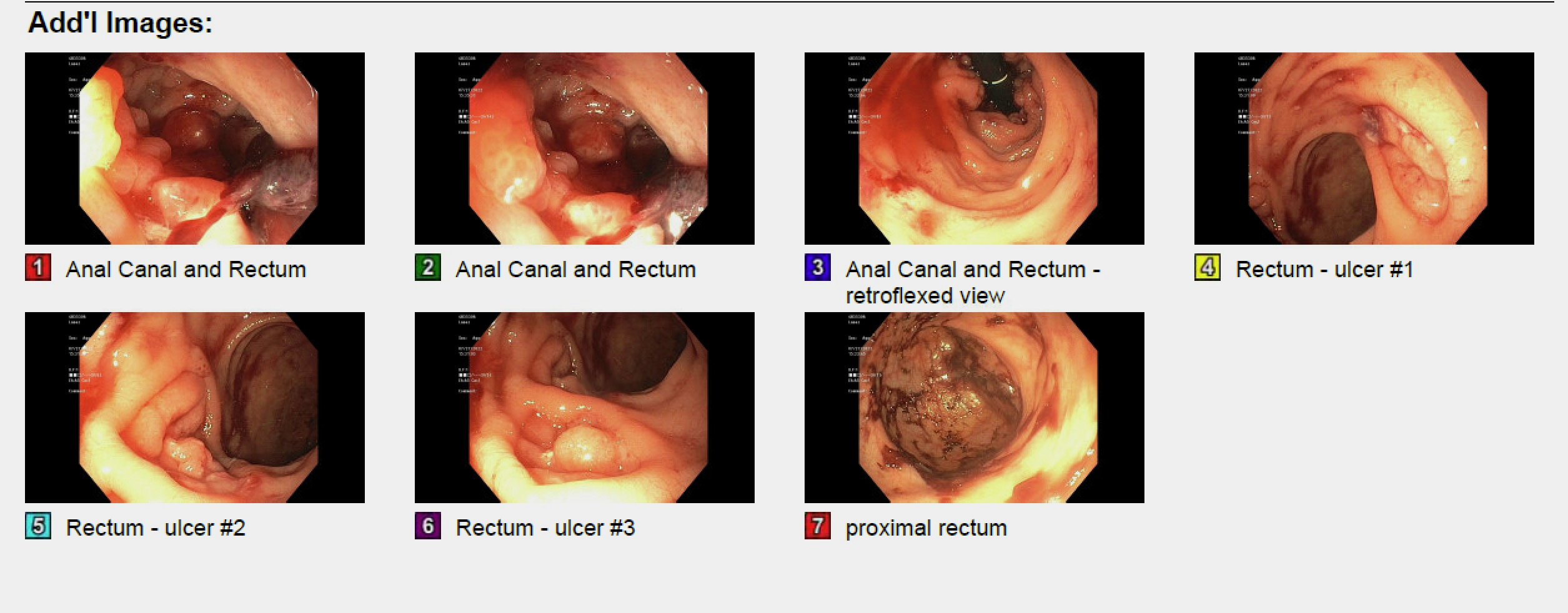
Case Presentation: A 58-year old male with no self-reported history presented to the hospital with hematochezia. Digital rectal exam revealed external hemorrhoids, shallow anal ulcers, a palpable internal rectal mass and frank blood. During his hospital course he required multiple blood transfusions for hemoglobin levels of 5-6 g/dL with ongoing rectal bleeding. CT and MRI of the abdomen and pelvis revealed an anal mass measuring 5.2 x 5.1 x 8.6 cm, involving the internal rectal sphincter with bilateral mesorectal, internal iliac and inguinal lymphadenopathy. Flexible sigmoidoscopy showed that the source of the bleeding was a circumferential, ulcerated and partially obstructing mass abutting the dentate line. There were also three 10mm ulcers in the distal rectum. Colorectal surgery performed an anoscopy for rectal biopsy and ligation of bleeding. Surgical resection with diverting ileostomy pending pathology of suspected rectal malignancy was initially considered. Biopsy specimens demonstrated anal tissue with chronic inflammation, ulceration and dense lymphoplasmacytic infiltration. While immunological staining was negative for infiltrating carcinoma cells, CMV and spirochetes, the histological features were suspicious of spirochetal infection. Testing for sexually transmitted infections demonstrated an RPR of 1:32, positive syphilis antibody testing, positive chlamydia trachomatis NAAT, positive HIV Ab and viral RNA. He subsequently admitted to being sexually active with men, participating in insertive and receptive oral and anal sexual intercourse and mentioned a history of treated syphilis. Thus, his ano-rectal lesions were attributed to rectal syphilis and lymphogranuloma venereum(LGV). He was treated for late latent/tertiary syphilis with weekly benazthine penicillin G for three doses, and for LGV with doxycycline. He was started on antiretroviral therapy for HIV. At an outpatient follow-up, the patient reported resolution in symptoms and a decision was made to repeat colonoscopy at a future visit to assess the ano-rectal mass.
Discussion: In 2019-2020, 43% of the total reported syphilis cases were among the “men who have sex with men”(MSM) population (1) . While rectal syphilis is a rare entity (2), it has been branded the “great masquerader”(3) due to its ability to mimic symptoms of a rectal malignancy. In the appropriate demographic setting, radiologic features of an ano-rectal mass with diffuse wall thickening might be suggestive of rectal syphilis (4). However, endoscopic findings from proctitis to pseudotumors and non-specific histology involving mononuclear cell infiltration suggesting inflammation warrants a broad differential diagnoses-solitary rectal ulcers, inflammatory bowel disease, chancroid, LGV, viral ulcers and cancer(5),(6). A thorough history with emphasis on patients’ social practices, albeit sensitive, can prevent mismanagement of rectal syphilis which resolves with medical management alone (3),(4),(5).
Conclusions: We highlight a case of rectal syphilis in a patient who presented with hematochezia. Rectal syphilis is a rare manifestation of the disease and can mimic rectal cancer, particularly if a large rectal mass is present. We acknowledge our initial anchoring bias in diagnosing rectal cancer. Our patient remained guarded throughout the admission. Improved physician-patient trust and a frank discussion of the patient’s social history early on may have revealed key elements of his sexual history sooner, aiding in accurate and timely diagnosis.