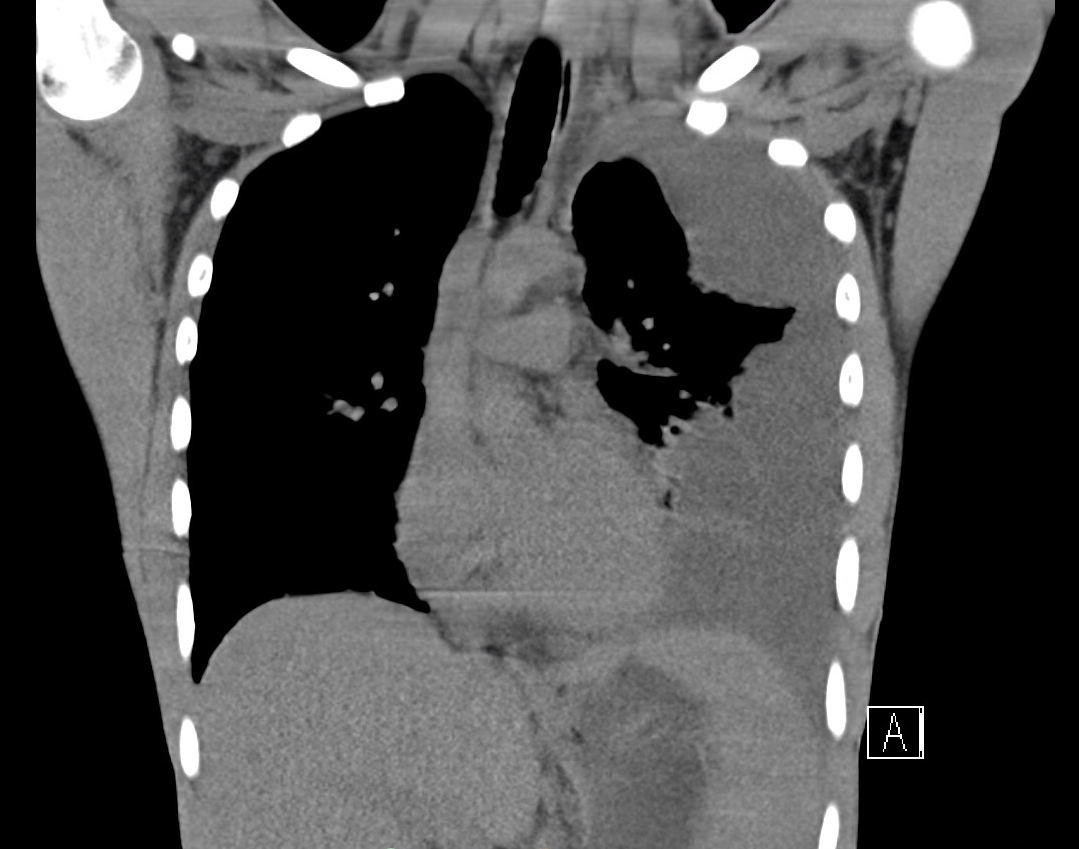
Case Presentation: A previously healthy 18-year-old male presented with a loculated pleural effusion. 10 days prior, the patient had sudden, acute, left sided anterior wall chest pain and shortness of breath. He reported night sweats, but no other symptoms. He was initially treated with doxycycline in the outpatient setting. Despite antibiotics, the symptoms worsened, and he sought care at an emergency department. Imaging obtained showed a loculated left pleural effusion with compressive atelectasis (Image 1). He was then transferred to our hospital for a higher level of care.Upon presentation, he was afebrile with a normal respiratory rate and work of breathing. On exam he was noted to have decreased breath sounds in the left lower lobe. He had a chest tube placed in the emergency department. On Hospital Day (HD) two, he was started on ceftriaxone and metronidazole empirically. Fluid studies from the pleural fluid were consistent with an exudative process without cytologic evidence of malignancy. Bacterial culture from the pleural fluid grew Neisseria species, which was further differentiated to Neisseria sicca. CT surgery was consulted, and on HD three performed a VATS with decortication. Cultures from the pleural rind also grew Neisseria sicca. Due to the unusual pathogen, immunologic work-up was undertaken and Infectious disease (ID) was consulted. Their recommendation was to discontinue metronidazole and continue ceftriaxone while inpatient with transition to amoxicillin-clavulanate (amox-clav) on discharge. The patient’s CH50, IgA, IgM, and IgG were within normal limits. Remarkably, IgE was undetectable. The patient continued to improve and was discharged on HD seven with amox-clav for a total course of three weeks. The patient was recommended to follow up outpatient with immunology.
Discussion: There are over 10 species of Neisseria that are known to colonize humans, and of them the non-meningitis and non-gonorrheal Neisseria species rarely cause disease. With knowledge that N. sicca is a natural habitant of the nasopharynx, and this patient’s selective IgE deficiency, it is likely this immunodeficiency played a role in pathogenesis. Notably, the patient denied any previous history of recurrent or atypical infections. To our knowledge, this is the first report of an empyema caused by any non-meningitis or non-gonococcal Neisseria species in IgE deficiency.
Conclusions: Empyema in a healthy patient should encourage further testing, particularly when dealing with an atypical organism. In this case, work up revealed an isolated IgE deficiency. This supports newer data emerging that IgE may have more of a role in the immune system’s ability to prevent bacterial infection than previously thought, and should be considered in the pathogenesis of unusual organisms. This case also brings to light the lack of guidelines for treatment of atypical Neisseria infections. Previous case reports have shown success with amox-clav, though standard guidelines are lacking.