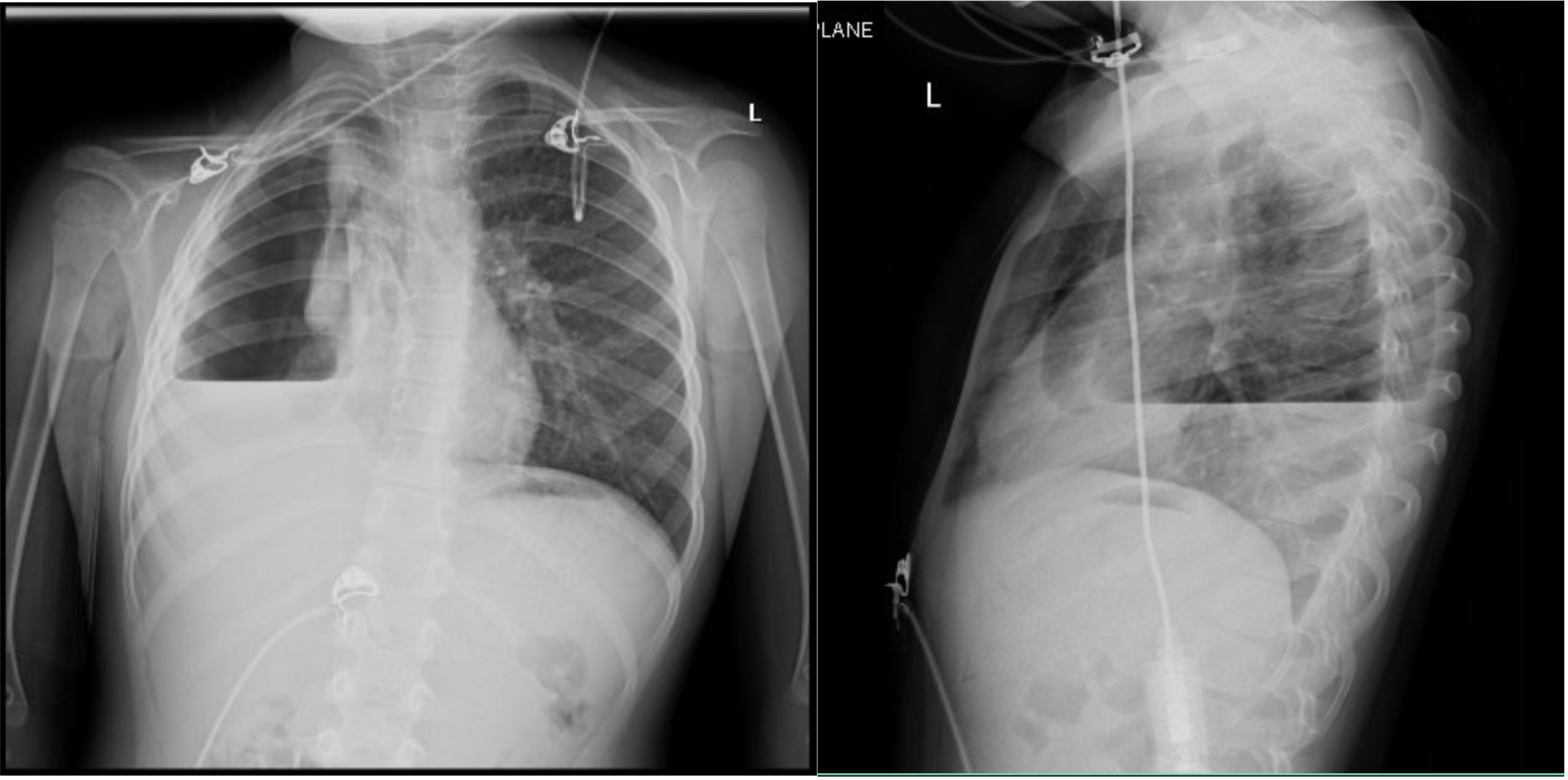
Case Presentation: A previously healthy 5-year-old female was transferred to our facility for increasing respiratory distress in the setting of a COVID-19 infection with suspected secondary bacterial pneumonia. Approximately five days prior, she tested positive for COVID-19 after developing a cough. She was treated with supportive therapy until parents noticed her “breathing heavily.” At the outside ED, she received a dose of Tylenol, Zofran, and Rocephin. CXR showed a RUL consolidation with air bronchograms and bulging fissures. She was started on Rocephin, azithromycin, and Decadron. Upon admission, repeat CXR was consistent with RUL consolidation and small bilateral pleural effusions. She was transitioned to Augmentin and discharged after three days. However, twenty-five days later, she returned after a follow-up CXR demonstrated right hydropneumothorax, despite resolution of symptoms. Pediatric Surgery placed a catheter in the right lung space, evacuating profuse blood. Pediatric Pulmonology was consulted and, along with Surgery, managed her condition with a chest tube. Serial CXRs showed gradual improvement of fluid and air collection. However, two weeks into treatment, she required a VATS with thoracoscopic adhesiolysis due to chest tube malfunction and worsening pneumothorax. Necrotic lung tissue was evacuated and a diagnosis of post-COVID necrotizing pneumonitis was given. She was monitored for ten days and, after twenty-three total days of treatment, was medically cleared for discharge with close follow-up.
Discussion: Pulmonary COVID-19 can be subdivided into four morphological stages, including (1) edema, incipient epithelial damage, and capillaritis/endothelialitis (day 0-1), (2) exudative diffuse alveolar damage (DAD) (days 1–7), and (3) the organizing (1 to several weeks) and (4) fibrotic stages of DAD (weeks to months). Despite the most frequent radiological manifestation being bilateral ground-glass opacities (GGO), as the disease progresses, GGO may disappear or evolve into frank consolidation. Pulmonary infarct should also be kept high on the differential diagnosis secondary to the microthrombotic nature of the disease. Based on the initial work-up, this patient’s diagnosis was secondary bacterial pneumonia with hydropneumothorax and possible empyema secondary to COVID-19. However, upon re-evaluation of her original CXR, the wedge shape consolidation was more consistent with a pulmonary infarct and subsequent hemopneumothorax.
Conclusions: COVID-19-induced hypercoagulopathy is a life threatening complication, even in children with an uncomplicated disease course. This atypical case of hemopneumothorax following COVID-19 infection highlights the importance of continual discussion and documentation of disease sequelae, as well as routine modification of prophylactic anticoagulation pathways.