Background: Patients with cancer diagnoses are known to have the highest likelihood of readmission to the hospital based on nationally available data. Reducing readmissions to the hospital has remained a national priority in healthcare quality, however it can be challenging to identify patients who are at highest risk for readmission to the hospital. Currently, our EHR system—Epic, generates a calculated prediction of likelihood of readmission for all patients. Our group hoped to better understand the reliability of Epic Readmission Risk Score in predicting the likelihood of readmission to the hospital in our population of cancer patients. Prior adjusted readmission prediction models, incorporating the Epic readmission score, have shown AUROC values ranging from 0.676 to 0.697.
Methods: Our group performed a retrospective review of all patients with cancer diagnoses who were admitted to our institution over a 1-year period from September 2021 to September 2022. Medical record data was obtained from Vizient reports as well as from the Epic EMR. A group of physicians reviewed the medical records of this patient population to classify the reason for readmission to the hospital and to verify the patient’s underlying tumor type.Our group also obtained the predicted Epic-generated readmission risk score at the time of the patient’s discharge from the hospital in order to be able to determine its accuracy in predicting which patients would return to the hospital within the 30-days following their initial hospitalization.
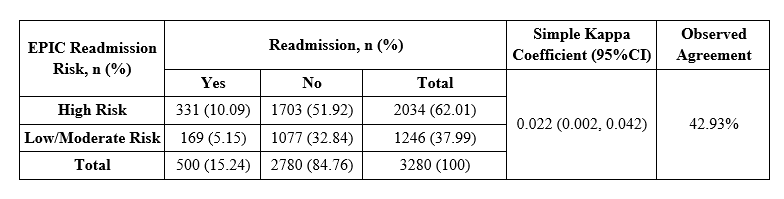
Results: During our study period from September 2021 to September 2022, a total of 3,292 patients with cancer were discharged from our institution. Of this group, 502 patients were readmitted to the hospital within 30 days of their discharge. The overall rate of readmission for our patient population was 15.3% .We found that the Epic readmission risk score showed low accuracy in predicting readmission to the hospital. Out of 3292 patients, 12 had no Epic risk score. Among the remaining 3280 patients, 331 readmitted patients had a high-risk Epic score (10.09%), and 1077 non-readmitted patients had a low to moderate-risk Epic score (37.99%) (Table 1). An observed agreement of 42.93% and a Kappa coefficient of 0.022 suggest that there was little agreement between readmission status and EPIC readmission risk score.Furthermore, Epic readmission risk score exhibited a sensitivity of 66.2%, a specificity of 38.7%, a PPV of 16.3%, a NPV of 86.4%, and an area under the curve (AUC) of 0.5247 (p = 0.036) when predicting hospital readmission (Figure 1), indicating a limited predictive accuracy.
Conclusions: In our patient population of cancer patients, the Epic readmission score as it is currently devised does not appear to help clinicians in distinguishing patients who are high risk for readmission to the hospital. Given the AUC of approximately 0.52 (vs. 0.5), the Epic readmission risk performs approximately as well as a flip of a coin to determining if a given patient will be readmitted to the hospital. Future efforts could focus on determining an alternate to the Epic readmission risk score in the cancer population.