Background: Documentation burden has been on the rise since the introduction of electronic health records (EHRs). Artificial Intelligence (AI) scribes use ambient documentation technology with the potential to mitigate documentation burden. Few studies have investigated the implications of AI scribes on hospital medicine providers’ workflow and patient interactions.
Methods: We conducted a stepped-wedge trial at 4 hospitals (2 academic medical centers, 2 affiliated community hospitals) in a single health care system to investigate the effects of an AI scribe on hospital medicine providers’ time allocation and the quality of patient-provider interaction. 9 hospital medicine providers were recruited from a larger operational pilot study and were each observed during 5 hospital admission encounters at two study time points. At time point 0, hospitalists were observed without the use of an AI scribe, and documentation time, direct patient care time and provider eye contact time with the patient were measured using time-motion methodology. Hospitalists were randomly selected in cohorts for AI scribe onboarding. All measurements were repeated within 1 month of onboarding at time point 1. Wilcoxon rank sum tests were performed to compare all outcomes at time point 1 to 0. Analyses were also stratified by provider gender, as prior literature demonstrate differences in documentation time and patient interactions. Analyses were performed using mixed effects linear regression, adjusted for fixed effects of study month, presence of a relative during the encounter, use of interpreter, and patient illness severity score and for random effect by provider. Outcomes in time point 2 (4-5 months after onboarding) will be evaluated once completed.
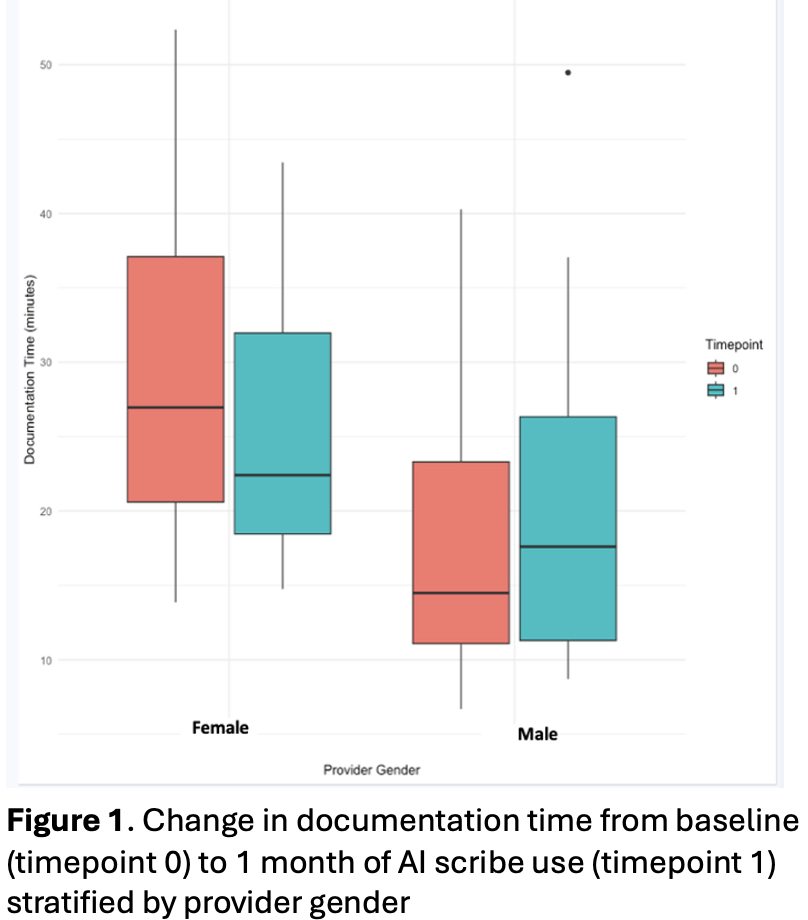
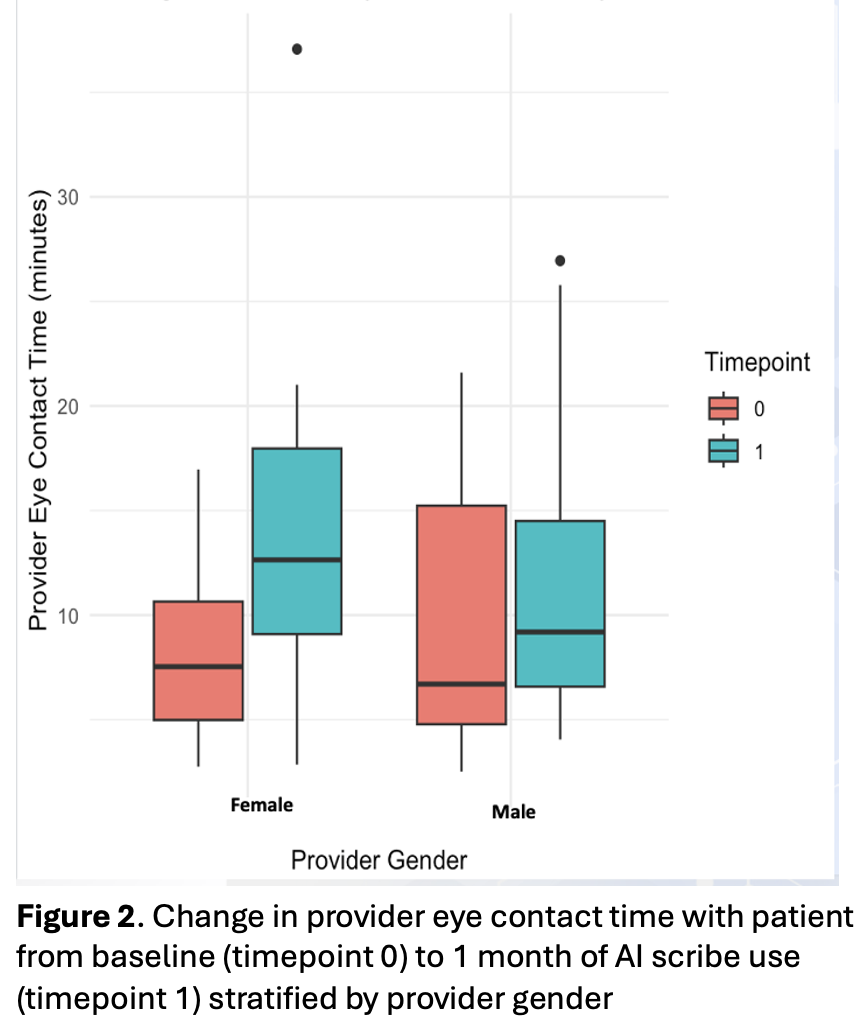
Results: At timepoint 0, all 9 providers were observed during 5 encounters each with a total of 45 observations. At timepoint 1, 5 providers were observed during 5 encounters and 4 providers were observed during 1-3 encounters, with a total of 32 observations. In timepoint 1 versus 0, when stratified by provider gender, there was a non-significant reduction in the median documentation time for female hospitalists from 27.0 to 22.4 minutes (p = 0.41), but a non-significant increase in median documentation time for male hospitalists from 14.5 to 17.6 minutes (p = 0.84) (figure 1). There was no change in direct patient care time. Median provider eye contact time with the patient increased from 7.53 to 12.64 minutes (p = 0.04) for females and from 6.70 to 9.19 minutes (p = 0.30) for males (figure 2), p = 0.06 for the entire cohort.
Conclusions: These preliminary results demonstrate the potential of AI scribes to reduce documentation burden, but that it may have varying effects for subgroups of hospital medicine providers. These differences, e.g. by provider sex would need to be substantiated in a larger adequately powered study and may be due to documentation practices prior to the introduction of the AI scribe, such as the use of dictation software. Additionally, there may be a learning curve associated with integrating new technology into clinical workflows, which further observations at timepoint 2 may demonstrate. The increase in provider eye contact time with patients for female and maybe male providers may suggest improved quality of patient-provider interactions. Further quantitative and qualitative work is needed to verify and better understand these results and understand the effects of AI scribes on provider experience and burnout, documentation quality, and patient experience.