Background: Patients who are frequently admitted to Medicine inpatient services comprise a distinct subset of readmitted patients about whom not much is known. A prior study collected data on characteristics of 153 frequently hospitalized patients. This was a follow-up evaluation to determine the categories of patients the original cohort belonged to, and to collect mortality data over a five year period in order better categorize distinct groups of frequently readmitted patients and to explore the varying mortality rates among the groups.
Methods: This was an observational study of frequently hospitalized patients defined as four or more non-elective admissions over a six-month period. Patients were adult inpatients on general medicine and medicine subspecialty services at a single large academic medical center. Based on clinical history and reason for admission, we retrospectively categorized each frequently hospitalized patient into one of three categories: 1) exacerbations of chronic disease (e.g. CHF, COPD), 2) terminal progression of end-stage disease, or 3) patients with frequent hospitalizations associated with chronic narcotic dependence. We additionally collected data about Charlson Comorbidity Indices (CCI) based on 19 comorbidities, and mortality for all patients, and age of death of each deceased patient over a five year period.
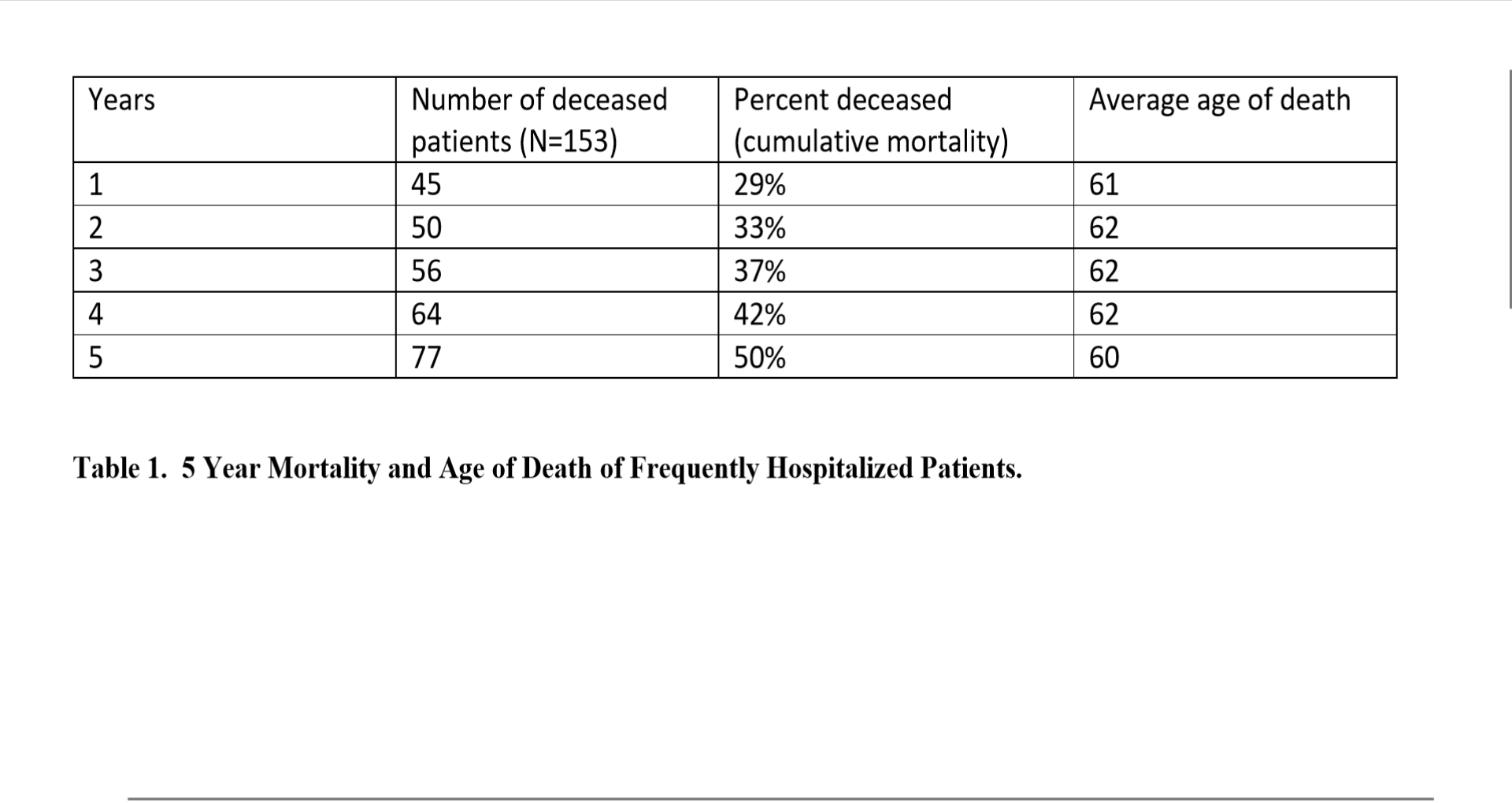
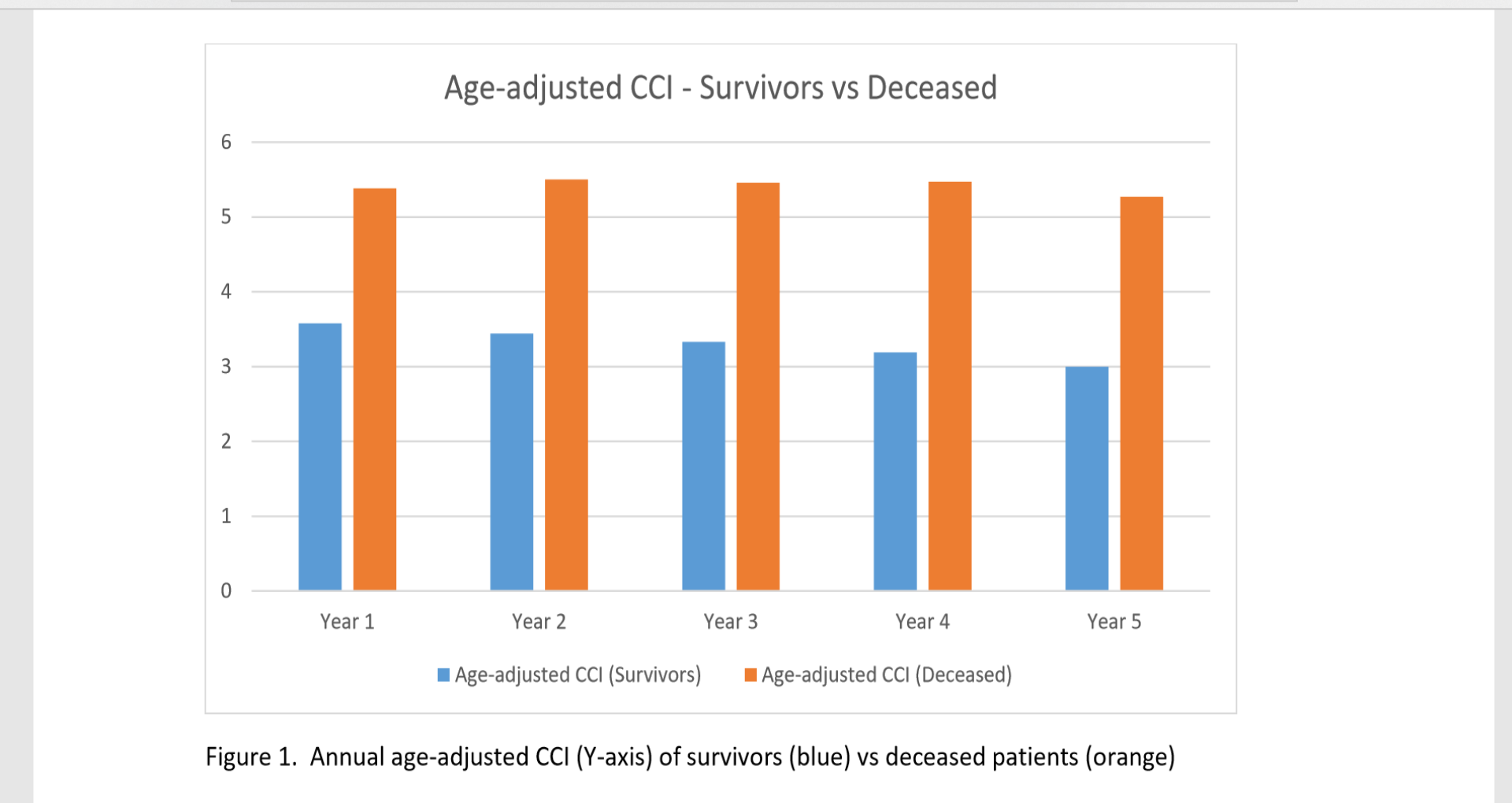
Results: The primary underlying condition contributing to recurrent hospitalizations was most often an exacerbation of a chronic medical condition (n = 52, 34%), followed by terminal progression of a medical condition (n = 45, 29%), and pain (n = 26, 17%), with the remainder (n = 30, 20%) not primarily fitting into one of the three categories. Aside from alcoholism – the primary underlying condition in six of the patients – other mental health disorders were typically not the reason for admission to the Medicine service, but rather as present as comorbidities. 29% of patients died within one year; a third (33%) were dead within two years, and half of all patients (50%) were dead within five years. This reflected a high 29% mortality within the first year, and an additional 5% annual mortality rate thereafter (Table 1). Over time, there was some cross over from the chronic exacerbation to terminal progression group, most notably for patients with CHF. The young average age of death (consistently 60-62 years over the 5-year period) was reflective of the high number of comorbidities in the terminal progression of disease group. Age-adjusted CCI scores ranged annually from 3.00-3.58 among surviving patients, vs 5.27-5.50 among deceased patients (Figure 1).
Conclusions: These findings point to distinct groups of patients who are frequently hospitalized. Those with progression of end-stage disease comprised one third of the group, and targeting that subset with palliative care referrals could help decrease readmission rates. Those with recurrent exacerbations of a chronic medical condition could be managed through telemanagement programs. Those with exacerbations of chronic pain could be addressed through collaboration with pain management specialists. Closer integration between hospitalist medicine services and palliative care and pain management services may be a means to address these needs. Among frequently readmitted patients, based on differences between survivors and deceased patients, an age-adjusted CCI score of 5 could be a valuable cutoff at predicting those who would benefit most from palliative care consultation regarding end-of-life goals and management.