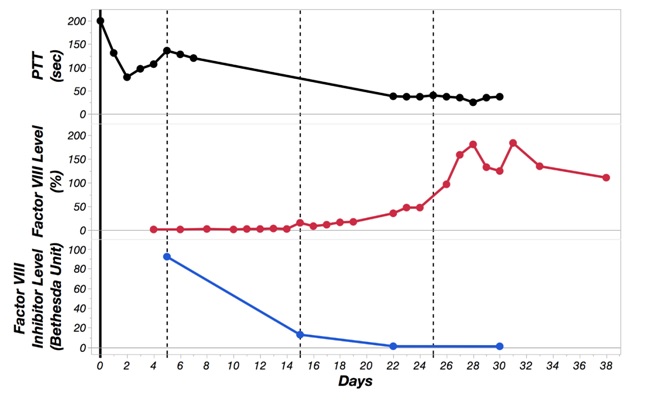
Case Presentation: 82-year-old man on chronic Warfarin presented for evaluation of spontaneous right lower extremity swelling with bruising. Workup showed hemoglobin of 9.5 g/dL, platelet of 286 K/µL, PT 47.4 seconds, INR 5.0, and PTT > 200 seconds. CT of abdomen and leg revealed intra-abdominal hemorrhage and subcutaneous hematoma of the right leg. Within the first 24 hours of hospitalization, patient had drop of hemoglobin down to 6.4 g/dL from acute hematochezia. Patient required multiple units of red cells and fresh frozen plasma along with vitamin K. Spontaneous bleeding initially was attributed to supratherapeutic INR level. However, further workup revealed incompletely corrected PTT mixing study with on ongoing prolonged PTT, concerning for acquired factor inhibitor. FVIII assay was 2% with significant inhibitor titer of 92 Bethesda Unit (BU). Patient was started on Prednisone 1mg/kg daily and Cyclophosphamide 1 mg/kg daily to eradicate inhibitor. Patient underwent malignancy workup that revealed a 2.6 cm anterior mediastinal mass concerning for thymoma. Hospital course was further complicated by development of left iliopsoas intramuscular hematoma. He required treatment with recombinant activated fVII to act as a bypassing agent and also with recombinant fVIII for hemostasis of iliopsoas bleeding. Immunosuppression resulted in increasing fVIII level and decreasing inhibitor titer (92 BU –> 13 BU –> 1.3 BU). Patient required prolonged rehabilitation due to severe weakness and sensory loss from iliopsoas hematoma and femoral nerve compression.
Discussion: Acquired Factor VIII inhibitor (also known as acquired hemophilia A or AHA) is a rare bleeding disorder caused by development of polyclonal inhibitory immunoglobulins G against fVIII, which blocks its interactions with other factors and prevents progression of normal coagulation cascade (1). Unlike congenital hemophilias, patient with AHA typically presents with large subcutaneous hematomas (>80%), muscle bleeding (>40%), and gastrointestinal bleeding (>20%) (4). Muscle bleeding in particular can lead to significant blood loss and vascular/nerve ischemia by compression as seen above. In a patient not on anticoagulation, finding of an isolated prolonged aPTT in setting of a significant bleeding event is suggestive of the diagnosis of AHA. Confirmatory labs for AHA include measurement of fVIII activity, mixing studies and Bethesda assay for inhibitor level (1). Disease process associated with AHA includes: malignancy (11.8%), autoimmune diseases (13.4%), pregnancy (8.4%), drugs (3.4%), and dermatologic diseases (1.4%) (2). Mortality in AHA from bleeding is high (9-22%), mostly due to intracranial, gastrointestinal, peritoneal, or intraoperative bleeding.(2)
The management of AHA focuses on the following goals: 1) Control and prevent bleeding; 2) eradicate inhibitor; and 3) treat underlying disease (4). Specific treatment strategies should be in consultation with hematologist at a facility with access to hemostatic agents and frequent FVIII monitoring.
Conclusions: Although AHA is rare with reported incidence of 1.5 case per million, it is important for general internists to promptly recognize and initiate appropriate management because failure to do so can result in high rate of morbidity and mortality.