Case Presentation: A 76 year-old African American female with no past medical history presented with new onset shortness of breath and substernal chest pressure of three week duration. She noted that she had been previously healthy without any issues prior to this incident. On presentation, the patient was afebrile and normotensive (125/76) but tachycardic (110 beats per minute) and tachypneic (24 breaths per minute). Physical exam revealed a patient in mild distress along with 1+ pitting edema and mild jugular venous distention (12 cm H2O). Significant labs included mildly elevated troponin (0.06) and BNP (314). All other labs including chemistries, complete blood counts, thyroid panel, and urine drug screen were negative. Chest x-ray showed mild bilateral pulmonary congestion and EKG revealed mild tachycardia and left atrial enlargement, but no ST or T segment abnormalities. The patient was admitted for new onset acute heart failure exacerbation and started on IV diuresis.
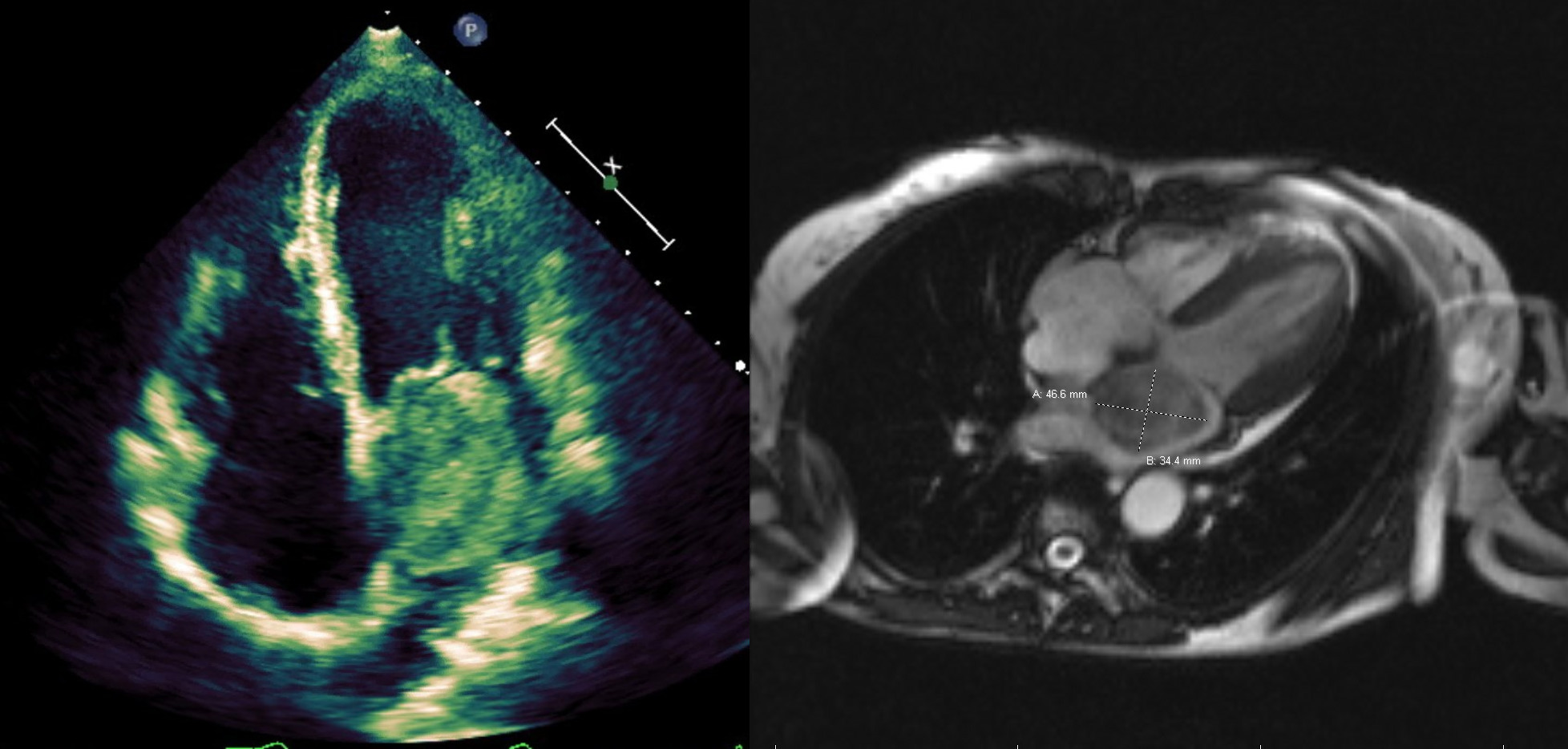
The patient noted no improvement in symptoms despite three days of escalating IV diuresis. Transthoracic echocardiography (TTE) revealed a 40% ejection fraction (EF), decreased left ventricular systolic function, and a large echogenic mass in the left atrium (LA), which was confirmed on transesophageal echocardiography (TEE). The mass was noted to be a heterogenic structure measuring 4.8×4.0 cm in the LA with a stalk (0.83 cm) extending from the interatrial septum. During diastole, the mass was noted to prolapse into the mitral valve without complete obstruction of flow. Cardiac MRI was significant for a 3.4×4.7cm pedunculated mass in the LA attached to the interatrial septum, consistent with a myxoma. After extensive discussion regarding the risks and benefits of surgical intervention were held with the patient, family, and members of the primary, cardiology, and cardiothoracic surgery services, myxoma excision was pursued. Pre-operative left heart catherization showed non-obstructive coronary artery disease of the right coronary artery. The patient then underwent successful atrial myxoma (39.3 grams) removal with repair of subsequent atrial septal defect with bovine pericardial patch. She tolerated the procedure well and was transferred to the intensive care unit for monitoring, where she was extubated within 24 hours. Pathology confirmed benign growth composed of primitive connective tissue cells in a myxomatous stromal background, consistent with a myxoma. The patient had steady clinical improvement and she was discharged to home 6 days after her operation. On follow-up, the patient noted complete resolution of symptoms. Repeat TTE at 3 and 12 months after discharge noted normal EF with no myxoma reoccurrence.
Discussion: The clinical manifestations of atrial myxomas are varied and often determined by their size, location, and mobility. However, the initial manifestation of atrial myxomas as acute heart failure is rare, especially in tumors that are smaller than 7cm in size. Even so, transient ball valve obstruction can occur, especially if the tumor is easily deformable or has a long pedunculated stalk as seen in our patient, leading to acute heart failure or even sudden cardiac death.
Conclusions: Left atrial myxomas must be considered as a differential diagnosis in elderly patients with new onset heart failure, especially in those who have no previous history of cardiovascular disease.
Management of atrial myxomas requires a multidisciplinary approach to facilitate shared decision making and promote patient centered care.