Case Presentation: A 69-year-old patient was referred to us by his PCP for subacute onset of confusion. Two months prior to presentation he was diagnosed with Focal segmental glomerulonephritis and had been on immunosuppressive therapy with Mycophenolate mofetil and Prednisone. He subsequently developed productive cough, and shortness of breath and was found to have a cavitary lung lesion on chest X-ray. Bronchoscopy done at an outside hospital revealed a right middle lobe cavitary pneumonia. Transbronchial biopsy was positive for Cryptococcus Neoformans and he was discharged home on PO fluconazole. Two weeks prior to presentation he developed confusion, lethargy and gait abnormality. On physical examination he had generalized anasarca, lethargy, ataxia, and had diffuse erythematous papules and plaques all over his torso. A Lumbar puncture was done at our hospital which revealed < 5 WBC, 123 mg/dl of protein and < 10 mg/dl of glucose. CSF PCR for Cryptococcus was negative. Given his history of immunosuppression, recent cryptococcal pneumonia, and focal neurological (ataxia, episodes of complex partial seizure) and cutaneous signs patient was presumptively treated for disseminated cryptococcal meningoencephalitis. Antifungal induction therapy was started with Liposomal Amphotericin B and Flucytosine. CSF fungal culture revealed Cryptococcus neoformans and confirmed our diagnosis of disseminated Cryptococcal meningoencephalitis. Cryptococcal titre on CSF was reported as 1:2560. Due to the lack of clinical response after patient had been on 12 days of Induction antifungal therapy, a second lumbar puncture was performed which revealed Glucose 16 mg/dl, Protein 144 mg/dl WBC 32 with 58% lymphocytes. Cryptococcal titers improved to 1:320 on the second CSF sample. Induction phase was continued for 2 weeks and then transitioned to PO fluconazole since serological improvement in Cryptococcal titer was noted. Two weeks after the second LP, the CSF fluid from the second Lumber puncture reported a new organism (initially misidentified as Rhodococcus), which was identified as Gordonia Bronchialis. Sputum sample was also positive for Gordonia Bronchialis. In the light of this additional information, patient was treated with IV Vancomycin and Ceftriaxone. Significant neurological improvement was noted with resolution of seizures, ataxia and confusion.
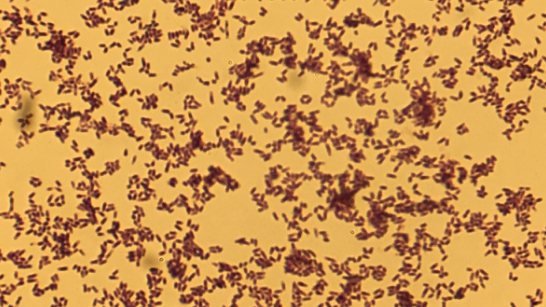
Discussion: Most patients with disseminated Cryptococcus infection are immunocompromised. It can take several weeks for fungal smear and culture results to be finalized, and delay in treatment approach can be avoided by keeping high clinical suspicion for disseminated cryptococcal infection. Gordonia species are gram positive, weakly acid-fast aerobic coccobacilli and belong to the actinomycetes family. It rarely causes infections in humans. Microbiologic diagnosis of Gordonia species is challenging, often leading to incorrect identification as Rhodococcus or Nocardia, as occurred in this case.
Conclusions: We report the first case of Gordonia Bronchialis meningitis in an immunosuppressed patient with disseminated cryptococcal meningoencephalitis. Microbiologic diagnosis and management of Gordonia species remains challenging in absence of any formal guidelines.