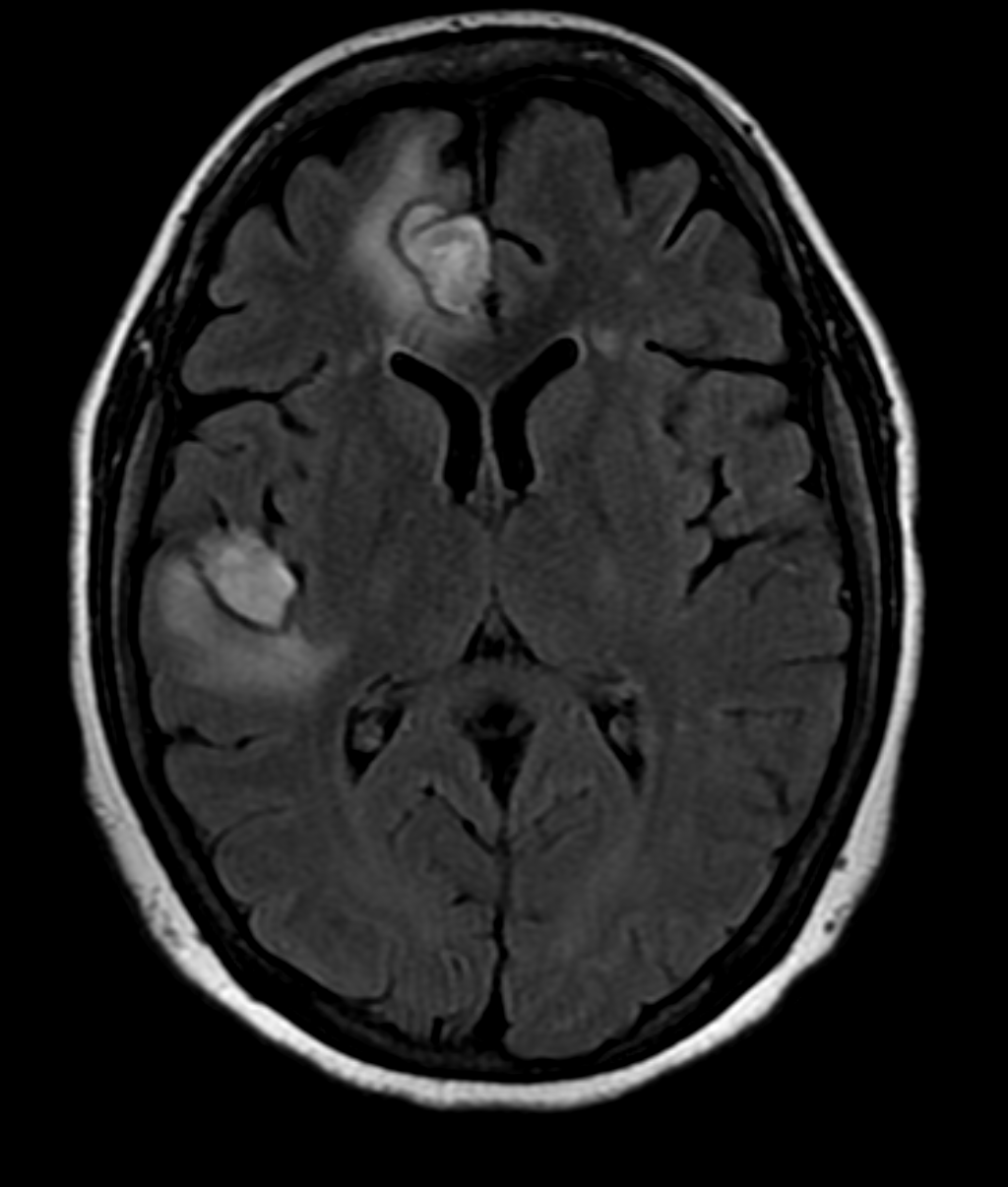
Case Presentation: : A 34-year-old female with history of migrainous headaches presented with complains of sudden onset, throbbing type of headache radiating to the back of the ear. This was associated with sudden loss of vision in the right eye. She also mentioned night sweats and unintentional weight loss in the last couple of months. She was diagnosed with grade 1 neuroendocrine tumor three months ago. On examination, she exhibited tenderness over the right temporal area and a decrease in visual acuity on the right eye. She did not show any signs of other focal neurological deficits. Initial laboratory investigations revealed thrombocytopenia and an elevated erythrocyte sediment rate. She was empirically treated with high dose glucocorticoids. Computed tomography (CT) scan of brain without contrast did not show evidence of intracranial hemorrhage. However, there were low density areas in the right frontal and temporal lobes suggesting possible demyelinating diseases, infarcts or metastasis. The patient was treated with high dose prednisone, which improved her visual acuity. This led us to do bilateral temporal artery biopsy which was negative for temporal arteritis. Magnetic resonance imaging (MRI) of the brain showed hemorrhagic areas which suggested the possibility of hemorrhagic intracranial metastatic disease, septic emboli or CNS vasculitis. Septic embolism was a distinct consideration, though this was excluded by negative transthoracic echocardiogram and blood cultures. The incidence of metastatic grade 1 neuroendocrine tumor is rare and seemed unlikely. We then proceeded to evaluate for vasculitis. Anti-nuclear antibody titers were highly positive as was Anti- double stranded DNA antibody. Complement 3 and 4 were low. Her presentation was consistent with SLE. On the next step, MR angiogram of brain confirmed small vessel hemorrhage in the right frontotemporal lobe suggestive of CNS vasculitis. High dose prednisone was continued for two weeks and a follow up MRI of brain showed improvement in the hemorrhagic areas. We concluded that the patient was suffering from CNS vasculitis secondary to SLE.
Discussion: SLE is a systemic autoimmune disorder that has many different presentations. Diagnosing CNS lupus is a challenging task and can often mislead the provider. Serological markers and imaging such as CT and MRI of brain, CT/MR and invasive angiogram are helpful in establishing the diagnosis. Brain biopsy is the gold standard to confirm the diagnosis, but remains poor in sensitivity. Initial therapy should be with high dose glucocorticoids. Other immunosuppressive agents such as mycophenolate, cyclophosphamide and rituximab may be used in combination.
Conclusions: Central nervous system (CNS) involvement in systemic lupus erythematosus (SLE) can manifest as psychosis, stroke, seizures and cognitive dysfunction. Such presentations of CNS lupus account for about 25% of the cases. In contrast, CNS vasculitis caused by SLE is rare and may pose as a diagnostic challenge when encountered.