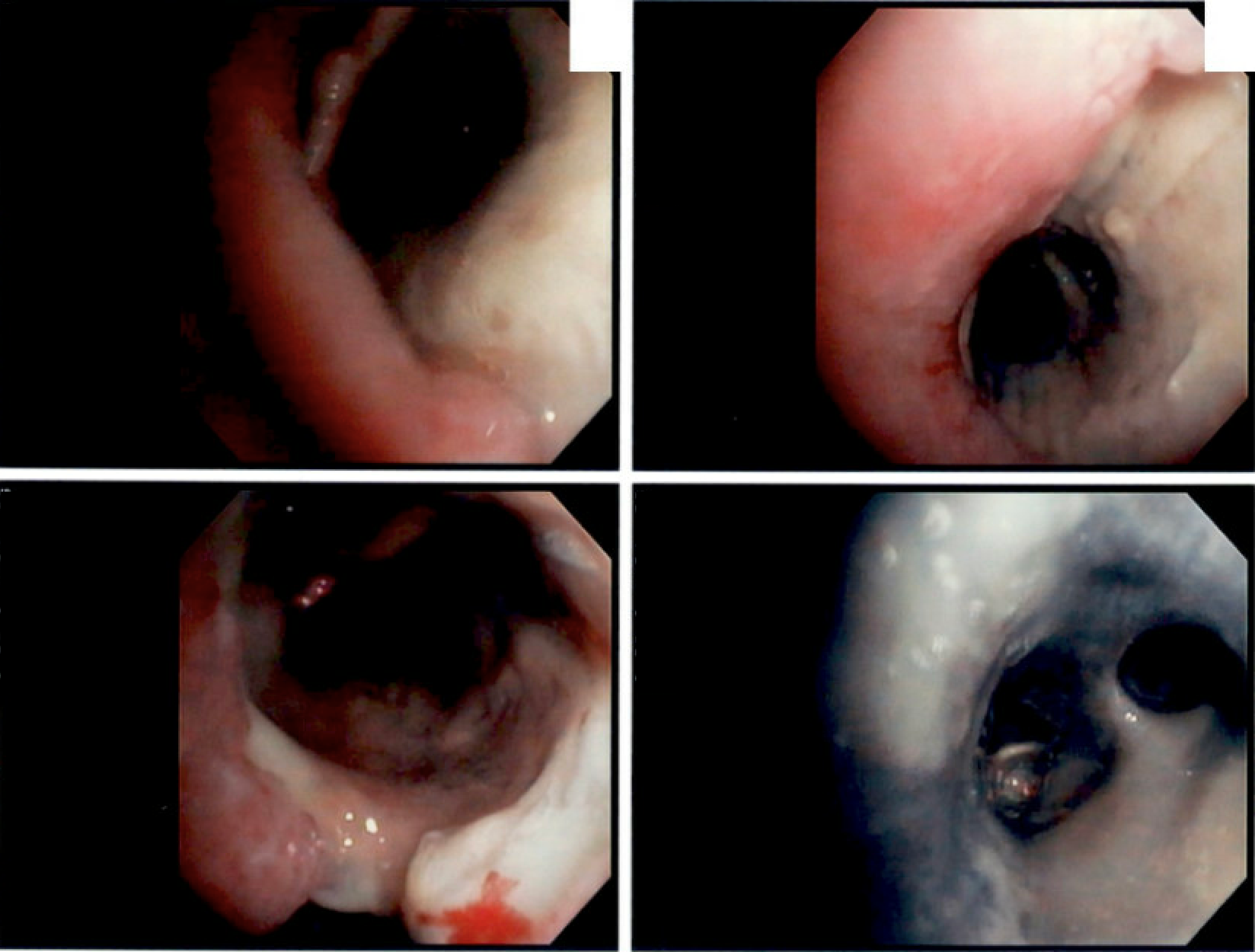
Case Presentation: A 50 year old female with history of type 1 diabetes mellitus, alcohol use disorder, and mood disorder was found down and unresponsive. She was intubated in the ED and admitted to the ICU for further management. Initial laboratory data was concerning for diabetic ketoacidosis, with a pH of 6.8, glucose 794 mg/dL, urine ketones 40 mg/dL and bicarbonate < 10 mmol/L. Toxic ingestion was considered; urine drug screen, salicylate, acetaminophen, and ethanol levels were all unremarkable. Treatment with insulin drip was immediately initiated with marked improvement in hyperglycemia and metabolic acidosis. An admission chest x-ray revealed right middle lobe consolidation. The patient was empirically treated with piperacillin/tazobactam and vancomycin with transition to amoxicillin/clavulanate for presumed community acquired bacterial pneumonia.The patient was eventually extubated after improved mental status, however, was unable to be effectively weaned off oxygen. She required 3-5 L O2, had transient fevers, and an increasing WBC count. Repeat chest x-ray revealed similar right middle lobe consolidation and new left perihilar congestion. There was concern for ventilator associated pneumonia; therefore piperacillin/tazobactam and vancomycin were re-initiated. Subsequent sputum cultures were obtained, and speciated with Rhizopus, Candida, and methicillin-susceptible Staphylococcus aureus (MSSA). CT chest revealed multiple cavitary lesions and ground glass opacities. It was unknown if the cavitary lesions were secondary to fungal vs bacterial etiology (MSSA), necessitating bronchoscopy. Gross findings on bronchoscopy showed copious yellow secretions with black mucosa concerning for necrosis (A). Endobronchial biopsy revealed ribbon-like non septate hyphae exhibiting wide angle branching, morphologically compatible with mucormycosis. The patient was diagnosed with pulmonary mucormycosis on hospital day 17.
Discussion: Common fungal genera found in human pulmonary mucormycosis infection includes Rhizopus, Mucor, and Rhizomucor. The fungus is found in decaying vegetation and soil. Pulmonary mucormycosis occurs when there is inhalation of fungal spores, which evade host immune function and results in infarction, necrosis, and contiguous spread among pulmonary and mediastinal tissue (2). Mortality rates for pulmonary infection can be up to 80 percent (2, 3, 5). Risk factors for pulmonary mucormycosis include hematologic malignancy, solid organ transplant, and corticosteroid use. In patients with diabetes mellitus, rhino-orbital-cerebral infection is more common, with unknown incidence of pulmonary infection (3, 4). Notably, CT maxillofacial did not reveal rhino-orbital-cerebral infection for this patient. The assumption for bacterial pneumonia is common in hospitalized patients, however, early recognition of fungal disease in diabetes mellitus/immunocompromised patients and early initiation of antifungal therapy can help to improve survival and outcomes (1).
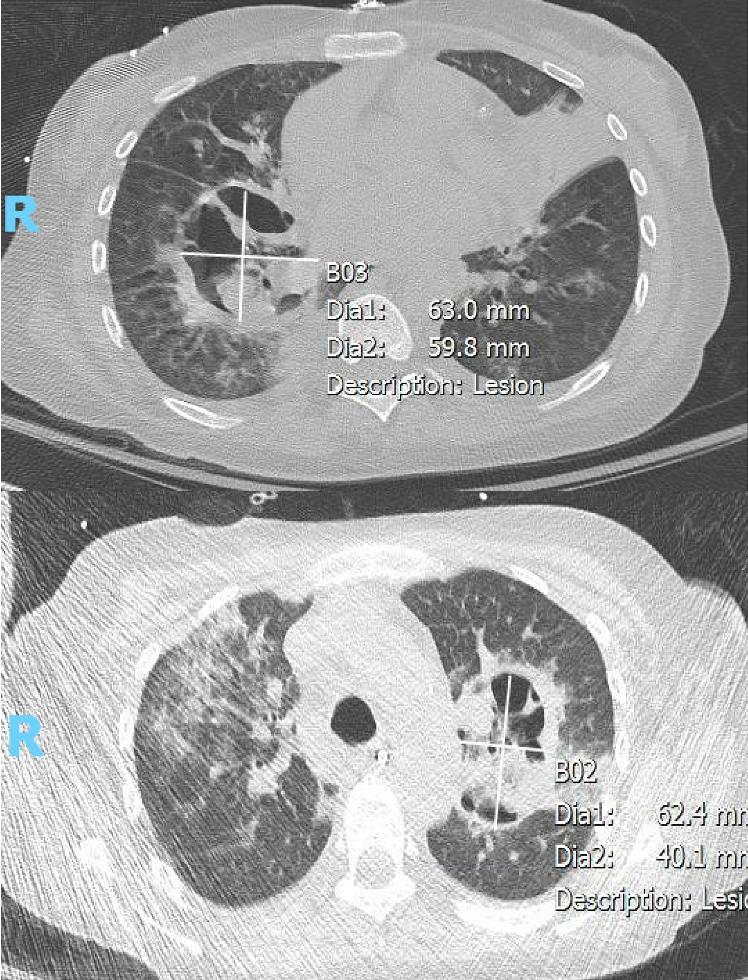
Conclusions: The patient was treated with liposomal amphotericin B for 7 days. Repeat CT chest on hospital day 22 showed interval enlargement of cavitary lesions to bilateral upper lobes (B). Due to bilateral infection, surgical resection was not a viable option. Given progression of disease while on antifungal therapy, there were no further options for escalation of care and a high likelihood of mortality from respiratory failure. The patient was discharged with comfort focused cares and died at home.