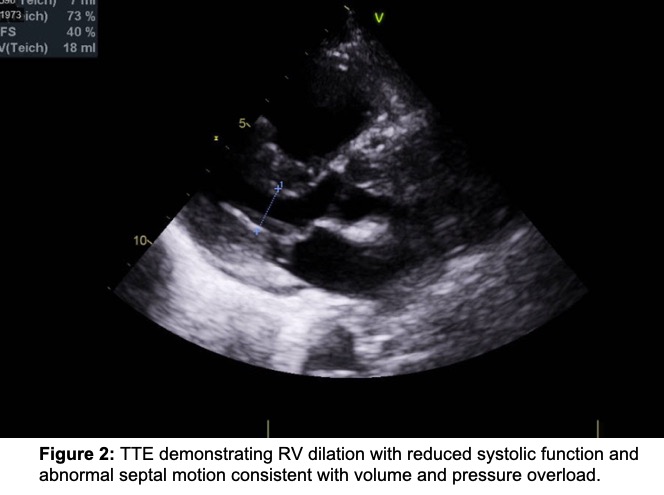
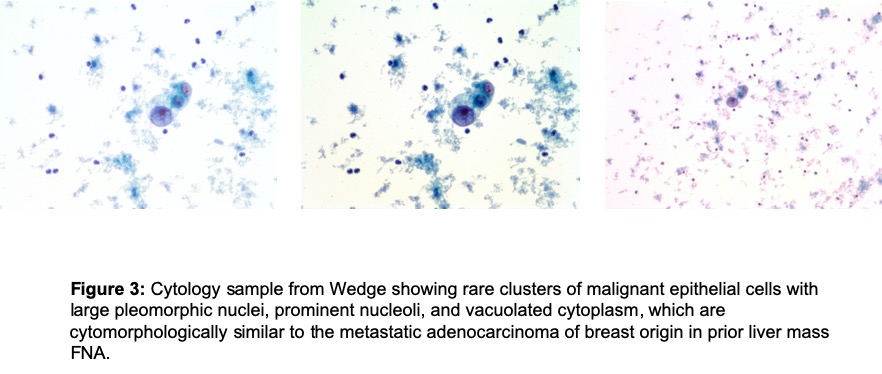
Case Presentation: A 45-year-old woman with a history of ER-/PR-/Her2+ breast cancer previously in remission, recently diagnosed with recurrent metastatic breast cancer pathologically and on imaging, presented to the hospital with multiple days of dyspnea and dry cough. Vitals were remarkable for hypoxia and tachycardia. Electrocardiogram showed sinus tachycardia without ischemic changes. Troponin and B-type natriuretic peptide levels were within normal limits. Complete blood count was notable for thrombocytopenia and peripheral smear showed schistocytes. Computed tomography angiography (CTA) of the chest was negative for pulmonary embolism (PE) and re-demonstrated stable multiple bilateral pulmonary nodules. She was admitted to the oncology service, and over the next 2 days, she became progressively more hypoxic and tachycardic. Transthoracic echocardiogram (TTE) demonstrated new right ventricular (RV) dilation with reduced systolic function concerning for acute RV failure. Repeat CTA of the chest was negative for PE. Emergent chemotherapy was initiated with pertuzumab, traztuzumab, and docetaxel. Right heart catheterization (RHC) demonstrated right atrial pressure of 10 mmHg, pulmonary artery pressure of 57/28 mmHg, pulmonary capillary wedge pressure of 8-10 mmHg, and Fick Cardiac Output of 2.4L/min consistent with pre-capillary pulmonary hypertension (pHTN). Cytology from the wedge were positive for malignant cells consistent with Pulmonary Tumor Thrombotic Microangiopathy (PTTM), and prednisone was initiated. Anticoagulation was not implemented due to thrombocytopenia. She was started on sildenafil, weaned to room air, and was discharged home on hospital day 18. Repeat TTE 3 months later showed resolution of the RV dilation and systolic dysfunction. Nine months after hospitalization she continues to do well.
Discussion: PTTM is a rare, fatal complication of metastatic cancer leading to hypoxia, pulmonary hypertension, and cor pulmonale. Small islets of malignant cells metastasize to small pulmonary vessels causing endothelial damage, activation of growth factors, cytokines, and coagulation cascade, resulting in fibrointimal remodeling and pHTN. Diagnosis is established histologically by tumor cells aspirated from wedge during RHC. Diagnosis is difficult because of shared symptoms with other disorders and the rapidly progressive course. Until recently, PTTM was considered universally fatal with most diagnoses made post-mortem. Optimal treatment is unknown, but case reports describe using a combination of chemotherapy, anticoagulation, pulmonary vasodilator therapy, and PDGF inhibition to target vascular remodeling. Our case demonstrates successful treatment of this rare, fatal disorder using chemotherapy, steroids, and pulmonary vasodilation. Unique to this case is the demonstration of complete reversal of RV failure on TTE after 3 months of treatment and overall clinical improvement.
Conclusions: PTTM is a rare, fatal cause of pHTN in patients with metastatic cancer. Underrecognition, shared clinical features and high mortality remain barriers to accurate and timely diagnosis. Optimal treatment may involve a combination of chemotherapy, anticoagulation, pulmonary vasodilation, and PDGF inhibition. To the best of our knowledge, our case represents the first demonstration of complete reversal of RV failure on TTE after treatment. Our case highlights the importance of early recognition and a multidisciplinary approach in treating this rare, fatal condition.