Case Presentation: A 63-year-old male with a medical history of hypertension presented with progressive vision loss over four months, with a one-month history of diffuse myalgias, increasing agitation, and altered behavior. He was an avid hunter with a history of frequent tick and deer fly bites. He presented to the emergency department with his wife due to progressive agitation, eventually requiring intubation for airway protection. Vital signs were significant for hypertension. Initial laboratory values were notable for C-reactive protein of 7.8 mg/dL and creatine phospho-kinase of 2695 mcg/L. Initial head computed tomography (CT) scan, magnetic resonance imaging (MRI) and lumbar puncture (LP) were negative. He was treated for aspiration pneumonia and extubated.However, he then developed worsening mentation, fever, and hypoxic respiratory failure requiring reintubation. A repeat brain MRI was negative. The patient developed myoclonic jerking, leading to multiple electroencephalograms, which demonstrated periodic discharges but no epileptiform abnormalities. Intravenous immune globulin and stress dose steroids were initiated without improvement. Subsequent LPs were negative for infectious etiologies. Tularemia IgG was elevated and the patient was started on empiric treatment while agglutination was pending. Cerebrospinal fluid samples were sent for Real-Time Quaking Induced Conversion Assay (RT-QuIC) and 14-3-3 testing. Autoimmune, paraneoplastic, and heavy metal screenings were negative. After one month of hospitalization, CJD labs returned with high suspicion of disease (positive RT-QuIC, tau protein > 20k, 14-3-3 > 160K).Considering the fatal diagnosis and high mortality rate, palliative care was proposed, and tularemia treatment was discontinued.
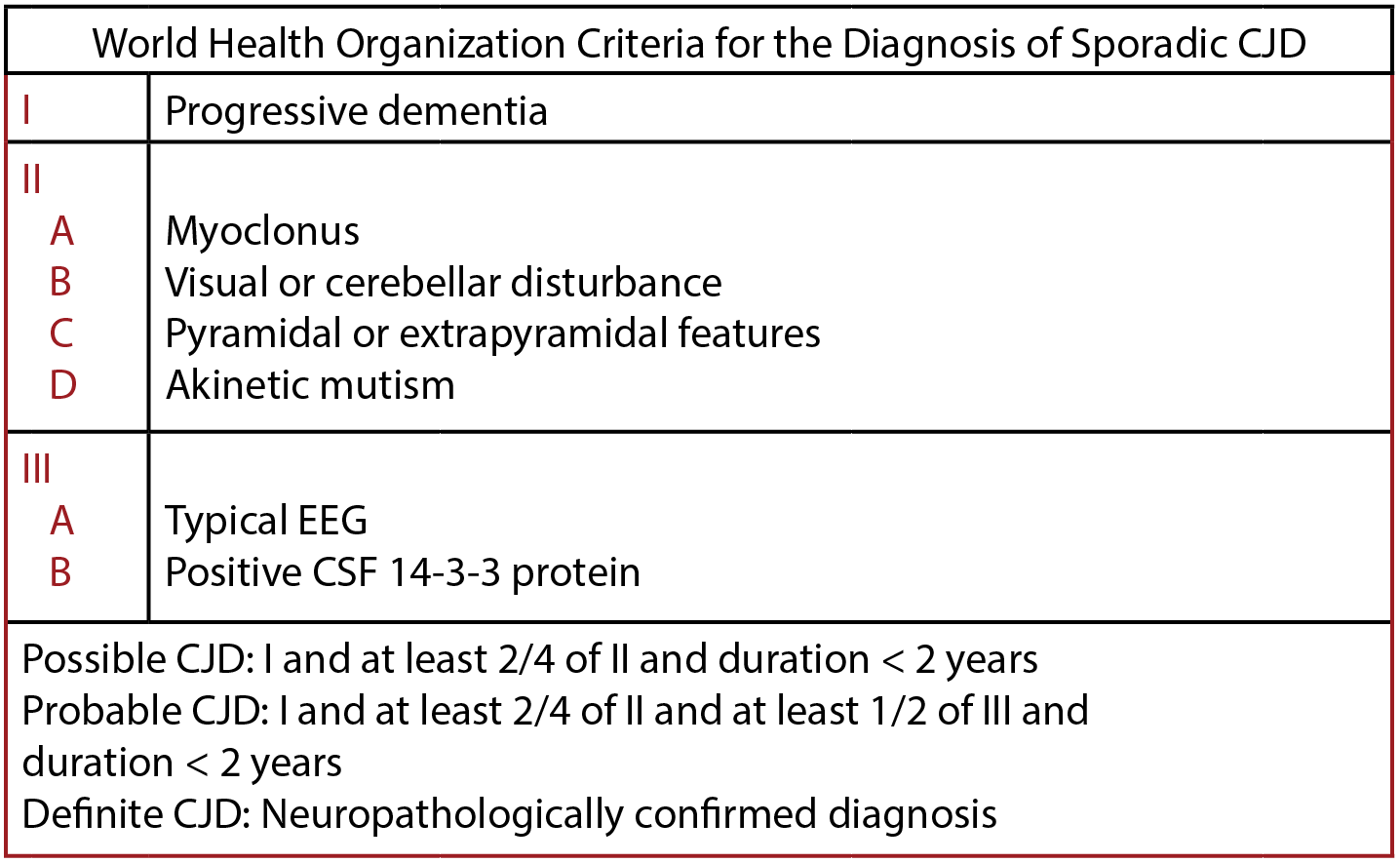
Discussion: CJD is a fatal neurodegenerative disease caused by the aggregation of misfolded glycoproteins known as prions. Prions from infected individuals are typically found in brain tissue or CSF. [3] Classically, CJD has four subtypes: sporadic, hereditary, variant, and iatrogenic. Sporadic CJD lacks a definite cause and comprises approximately 85% of cases with a mean age of onset of 62 [4] . Diagnostic testing for CJD typically includes a 14-3-3 protein assay and Rt-QuIC with a turnaround time of 7-17 days [5]. Delay in diagnosis leads to empiric treatment of confounding and curable etiologies. This case serves as a reminder of the potential for diagnosis of CJD in patients presenting with nonspecific symptoms or without concrete source in their history and physical. The development of readily available screening mechanisms or diagnostic tests that allow for a rapid diagnosis could minimize patient end-of-life morbidity, costs incurred by the family, and the potential iatrogenic spread of this fatal disease [6].
Conclusions: Creutzfeldt-Jakob Disease (CJD) is a rapidly progressive neurodegenerative disorder with an inevitably fatal outcome. The disease itself is rare with the CDC estimating the worldwide incidence of CJD to be 1-2 cases per million population. Magnetic resonance imaging (MRI) is the most sensitive test when diagnosing CJD, with studies showing 83-94% sensitivities.