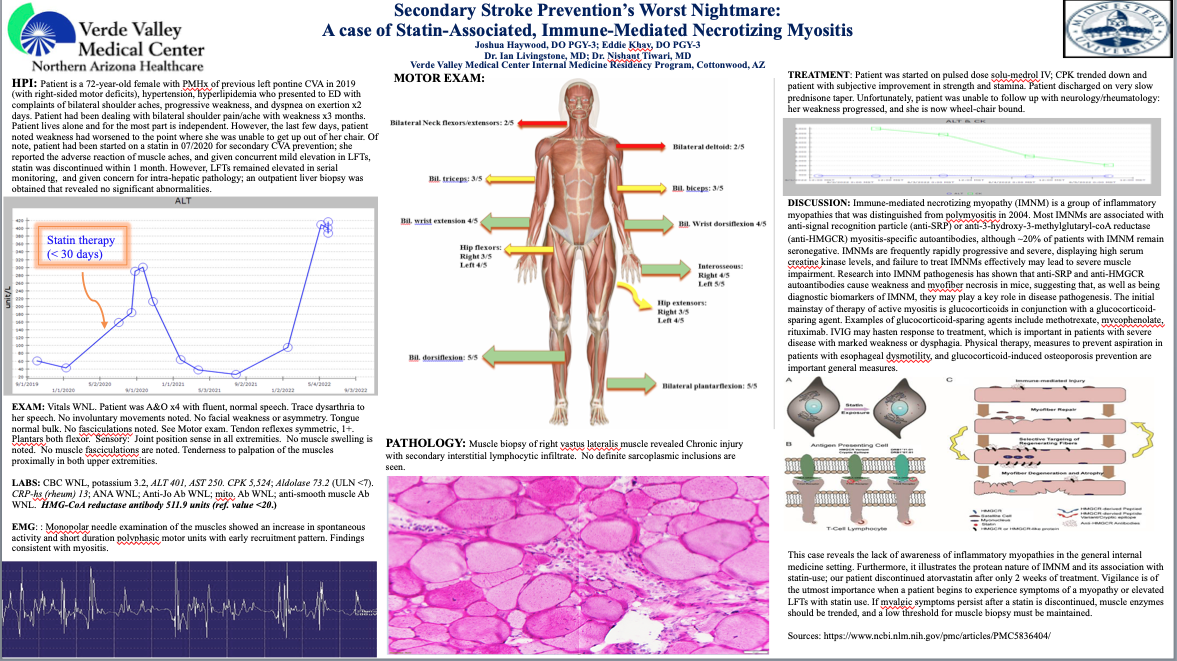
Case Presentation: This case describes a 72-year-old female with previous left pontine cerebrovascular accident (CVA) in 2019, hypertension and hyperlipidemia who presented to the Emergency Department with worsening bilateral shoulder pain and progressive weakness. Two years prior, statin therapy was started for secondary CVA prevention, however, the statin was discontinued because the Patient developed muscle aches associated with mild elevations in LFTs and normal outpatient liver biopsy findings. Physical examination revealed an alert and oriented elderly female with mildly dysarthric speech, symmetrical tendon reflexes, decreased muscle strength and tenderness of bilateral proximal muscles, and distal muscle strength sparing; there were no fasciculations. Labs showed ALT 401, AST 250, CPK 5524, aldolase 73.2. Neurology performed electromyography with findings consistent with myositis. Given concerns for polymyositis, a pulse dose of IV Solu-Medrol was initiated with improvement of strength and mobility. Additional diagnostic testing was performed and sent out with results returning after patient had been discharged. A muscle biopsy of right vastus lateralis showed chronic injury secondary to interstitial lymphocytic infiltrate and elevation of HMG-CoA reductase antibody at 511.9U (ULN < 20). Unfortunately, the patient was lost to follow up with neurology/rheumatology and her weakness progressed, leaving her wheelchair bound.This patient received only two weeks of statin therapy, and quickly developed myalgia, weakness and elevated LFTs, however her diagnosis of IMNM was not made until about 2 years later. In statin-associated anti-HMGCR IMNM, statin withdrawal and corticosteroids alone are usually not sufficient, and may require adjunctive IVIg and immunosuppressants.
Discussion: Immune-mediated necrotizing myopathy (IMNM) is a relatively novel clinical entity among autoimmune myopathies characterized by severe proximal muscular weakness, elevated serum muscle enzyme levels, autoantibodies and inflammatory muscle biopsy. There are two autoantibodies that have been associated with IMNM: signal recognition particle (SRP) and 3-hydroxy-3-methylglutaryl-coenzyme A reductase (HGMCR), although ~20% of patients with IMNM remain seronegative. Autoimmune myopathies are a rare disease; however, it can rapidly progress to debilitating weakness which highlights the importance for early recognition and initiation of aggressive immunosuppression. Statin exposure is often linked to anti-HMGCR IMNM and can develop even after cessation of statin therapy. Pathogenesis is hypothetical, but may be due to over-expression of HMGCR in genetically susceptible individuals which subsequently leads to the development of autoantibodies against HMGCR.
Conclusions: The case highlights a lack of awareness of inflammatory myopathies in the general internal medicine setting, which emphasizes the importance of vigilance in patients with statin-induced myalgias, allowing for a low threshold for thorough workup and aggressive treatment to prevent neurologic deterioration.