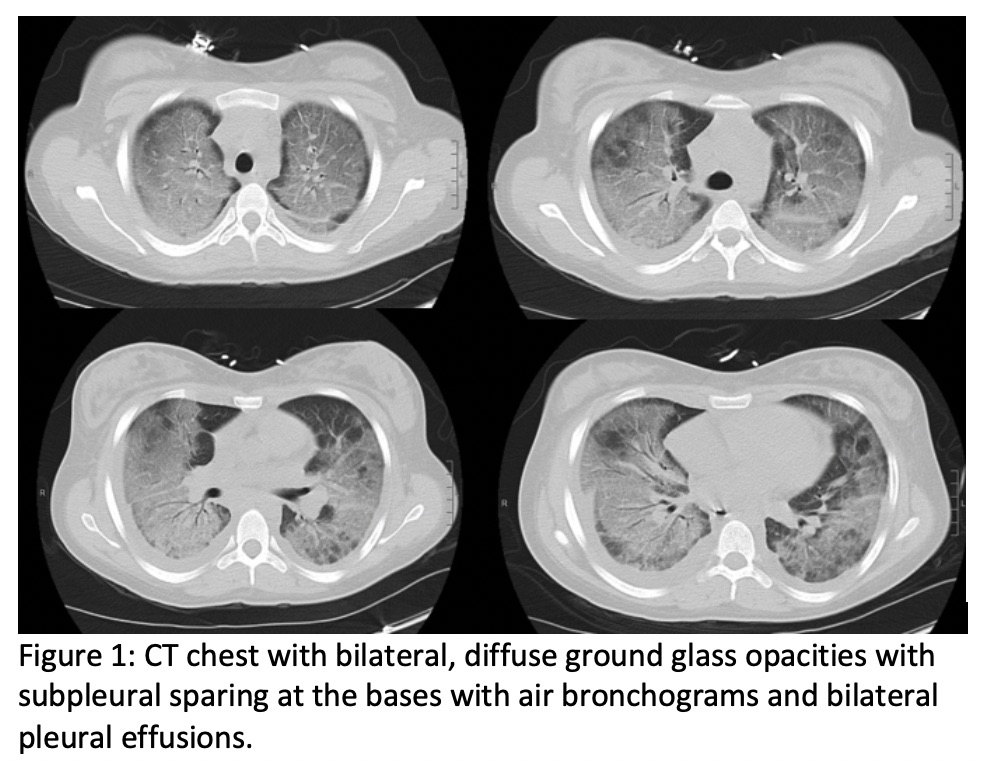
Case Presentation: A 19 year old female with history of marijuana use presented with subacute, progressive shortness of breath. Productive cough began two weeks prior to presentation. She was diagnosed with atypical pneumonia and received azithromycin from her outpatient provider. After two days without improvement in symptoms, she presented to a nearby hospital with acutely worsening shortness of breath. Social history was significant for three years of marijuana inhalation using vaporizers such as Juul and tetrahydrocannabinol(THC)-containing cord product. Notably, patient reported switching her inhalant two months prior to presentation.She was discharged with azithromycin from an outside hospital emergency department and then her primary care doctor. After failing two courses of azithromycin, she subsequently re-presented to the emergency department with worsening shortness of breath and hypoxia to 79% on room air. She required bilevel positive airway pressure and high flow nasal cannula. Her initial labs were negative for lactate dehydrogenase, HIV, and urine legionella antigen. Rheumatologic labwork was found to have an undetectable ANA. Chest x-ray and computed tomography(CT) of chest were notable for severe bilateral, primarily central, interstitial infiltrates with subpleural sparing at the bases with pleural effusions (Figure 1). The patient was treated with intravenous solumedrol with eventual prednisone taper. Bronchoscopy was deferred as the hypoxia rapidly resolved.
Discussion: Vaping induced lung injury is a rare but deadly condition with increasing incidence over the last year. E-cigarettes are becoming popular among younger otherwise healthy patients putting them at risk of lung injury given the uncertain composition of most of their aerosol contents. Over the last several years, the majority of affected patients are less than 35 years old and male. Hospitalists must be vigilant in their evaluation of dyspnea complaints with this new pulmonary threat facing patients who vape. Vaping-associated lung injury should be high on the differential diagnosis of any patient admitted to the hospital for dyspnea with any history of vaporizer use, especially if used 90 days prior to symptom onset. Our case was unusual in that an otherwise healthy female patient with a long history of using vaporizers presented suddenly with acute hypoxic respiratory failure. While there are no definitive diagnostic imaging criteria for vaping-associated lung injury, 100% of cases reported in the literature were associated with bilateral opacities, similar to this patient suggesting that further invasive testing with bronchoalveolar lavage may not be required for diagnosis. Similarly no definitive treatment has been determined for this condition, however, it is likely best treated with cessation of e-cigarette use. In this case, the patient was also continued on a prednisone taper with Bactrim PJP prophylaxis and outpatient pulmonology follow up.
Conclusions: The diagnosis of vaping-associated lung injury should be highly considered by hospitalists for any patient presenting with acute hypoxic respiratory failure and bilateral opacities on CT scan, who has any history of e-cigarette or vaporizer use.