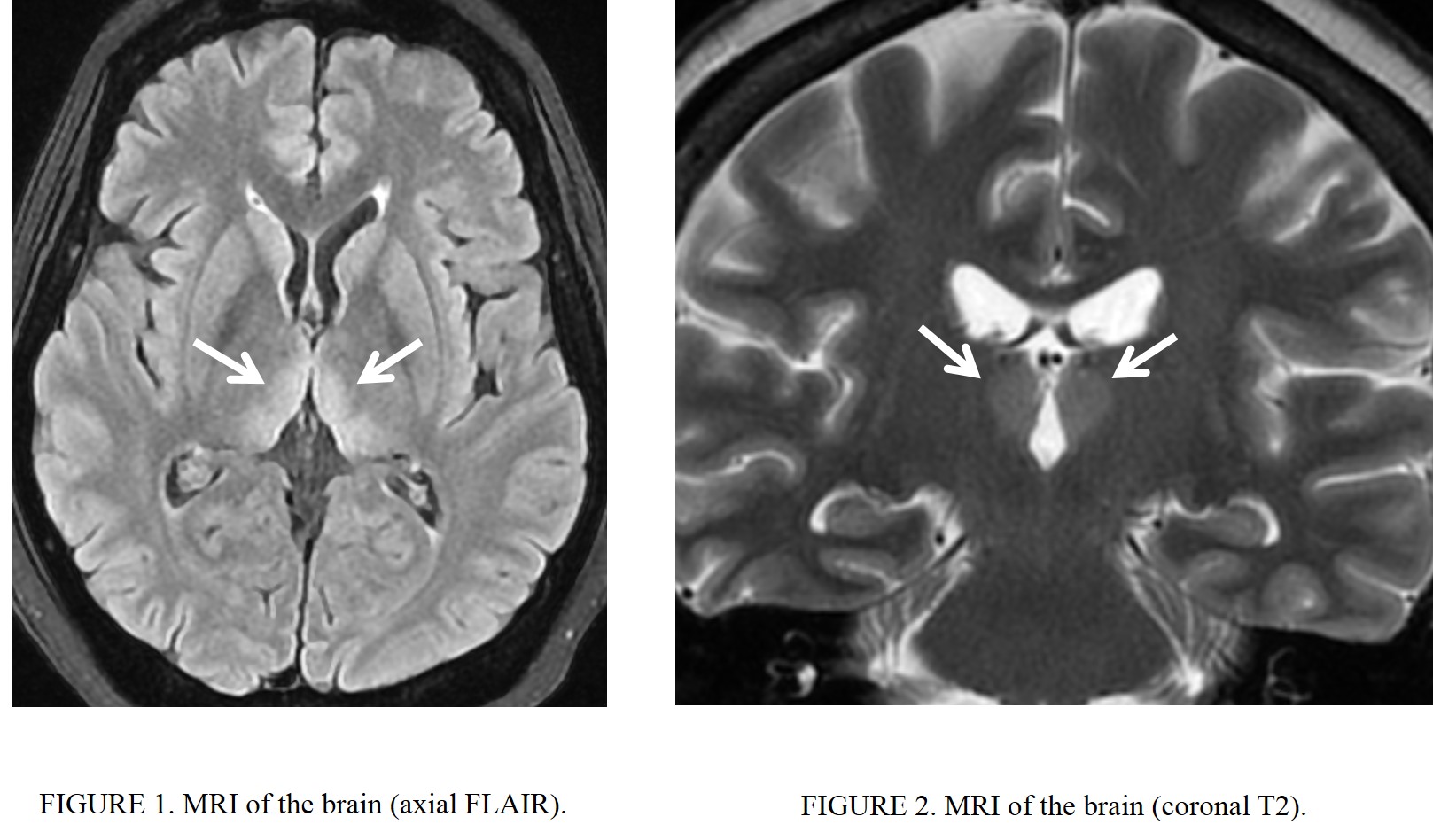
Case Presentation: A 53 year-old female with poorly differentiated gastric adenocarcinoma metastatic to the lungs was hospitalized with repeated vomiting for almost two months. She reported vomiting with every meal but without abdominal pain. IV ondansetron, metoclopramide, and prochlorperazine provided only minimal improvement in the hospital. Esophagogastroduodenoscopy showed gastric body obstruction due to a large ulcerating cancer, and a gastric stent was placed as treatment. In the morning following the procedure, the patient was somnolent, minimally interactive, and with a disconjugate gaze and bilateral abducens nerve palsy as well as both horizontal and vertical nystagmus. A stroke code was called, but no acute stroke was found on a STAT head CT scan with contrast. An MRI of the brain with and without contrast was done a few hours later and showed bilateral symmetric hyperintensity in the dorsomedial thalami raising concerns for autoimmune encephalitis versus Wernicke’s encephalopathy. High-dose IV thiamine was initiated, and the patient’s mental status and other neurologic symptoms subsequently improved rapidly. This supported a diagnosis of Wernicke’s encephalopathy, and it was assessed that malnutrition in the setting of cancer and poor PO intake of thiamine (vitamin B1) was the cause.
Discussion: Wernickes’s encephalopathy develops in a setting of thiamine (vitamin B1) deficiency. Thiamine is critical for the metabolism of carbohydrates, and it also plays a role in muscle contraction and the conduction of nerve signals. Wernicke’s encephalopathy classically presents with the triad of ophthalmoplegia, ataxia, and encephalopathy. It may be challenging to diagnose Wernicke’s encephalopathy because not all of the classic triad is presented in many cases. Although it is traditionally associated with chronic alcoholism, there have been case reports of Wernicke’s encephalopathy in malignancy. Increased thiamine consumption due to the rapid growth of cancer cells and chronic malnutrition due to nausea and anorexia from chemotherapy or malabsorption syndrome have been proposed as reasons. Wernicke’s encephalopathy should be considered in patients with advanced GI tract cancer with acute neurological symptoms, particularly in those who suffer from chronic malnutrition and poor oral nutrition. MRI of the brain can aid in diagnosing Wernicke’s encephalopathy, and typical MRI findings include symmetrically increased abnormal signal intensities of the mammillary body, medial thalamus, hypothalamus, and midline brain. Wernicke’s encephalopathy can be partially or fully reversed with prompt thiamine supplementation. Without proper treatment, Wernicke’s encephalopathy can be life-threatening and potentially cause enormous disability. A small number of patients can progress to Korsakoff psychosis which often requires institutionalization, severely diminishing the quality of life.
Conclusions: Wernicke’s encephalopathy is a neurologic disease caused by thiamine (vitamin B1) deficiency. It is clinically characterized by ophthalmoplegia, ataxia, and acute confusion. Here we present a unique case of Wernicke’s encephalopathy associated with gastric outlet obstruction in the setting of advanced poorly differentiated gastric adenocarcinoma. It is important to consider Wernicke’s encephalopathy in gastric cancer patients with acute neurological symptoms. High-dose parenteral thiamine supplementation should be started as soon as Wernicke’s encephalopathy is suspected.