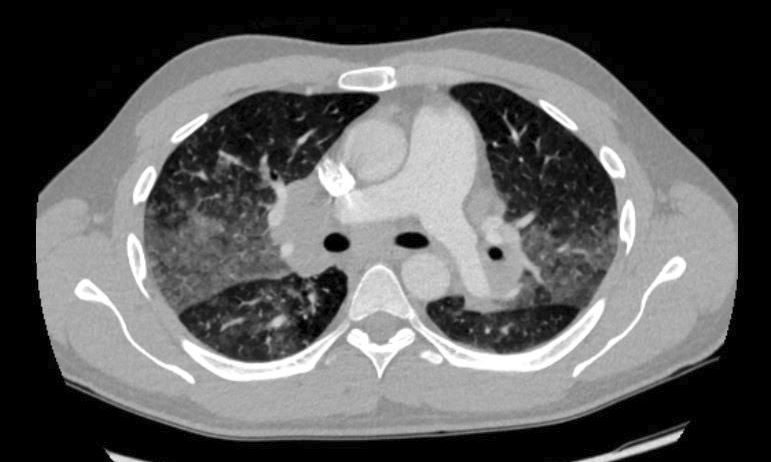
Case Presentation: A 28-year-old man with ulcerative colitis treated with adalimumab presented with headache, fever and sinus symptoms that progressed over two weeks to neck stiffness, “clouded” thinking, and intermittent left arm and facial numbness. On physical examination, he had normal cardiorespiratory findings. He had mild nuchal rigidity but an otherwise normal neurologic examination. CT head was normal. Cerebrospinal fluid (CSF) evaluation was consistent with aseptic meningitis (CSF protein 86 mg/dl, leukocytes 80 cells/cmm with 97% lymphocytes). CSF HSV PCR and a nasopharyngeal respiratory viral PCR panel were negative. MR brain and cervical spine were also unremarkable. A few days later, he developed worsening fever, dyspnea, severe bilateral chest pain, and hypoxia. CT chest revealed extensive diffuse ground-glass opacities with bulky enlarged bilateral hilar lymph nodes (figure) and splenomegaly. He was treated with broad-spectrum antibiotics. A transbronchial biopsy of a mediastinal lymph node showed necrotizing granulomas with negative tuberculosis (TB) and fungal stains. Flow cytometry testing and CSF cytology were negative for lymphoma. Fungal infection and sarcoidosis topped the differential diagnosis. A thorough infectious work-up was negative including Quantiferon TB, fungal culture, fungal serology, and a β-d-glucan assay. Due to clinical worsening and having sufficiently excluded infectious causes, he was started on steroids for probable sarcoidosis with prompt improvement in headache, dyspnea, chest pain and hypoxia. Tumor necrosis factor (TNF) inhibitor therapy was felt to be the most likely cause of sarcoid-like granulomatosis presenting with aseptic meningitis, pulmonary infiltrates, mediastinal/hilar lymphadenopathy, and splenomegaly. Adalimumab was discontinued. A few months later, he had completely recovered.
Discussion: Adalimumab is a recombinant human monoclonal antibody against TNF-α. TNF inhibitors are used to treat a variety of autoimmune and inflammatory diseases including sarcoidosis. However, several cases of sarcoid-like granulomatosis have been reported in patients treated with etanercept, infliximab, and adalimumab. While the molecular mechanisms to explain such a paradoxical effect are not fully understood, a few hypotheses have been proposed. TNF inhibitors are associated with an increased risk of developing serious infections such as TB, histoplasmosis, listeriosis, and pneumocystis, as well as lymphoma. Infectious causes of granulomatoses, particularly TB and histoplasmosis should be ruled out before making a diagnosis of sarcoidosis.
Conclusions: Hospitalists should be aware that TNF inhibitors can rarely cause sarcoid-like granulomatosis. While most of these cases present with pulmonary sarcoidosis, neurosarcoidosis can also occur. Discontinuation of the anti-TNF agent is necessary for recovery.