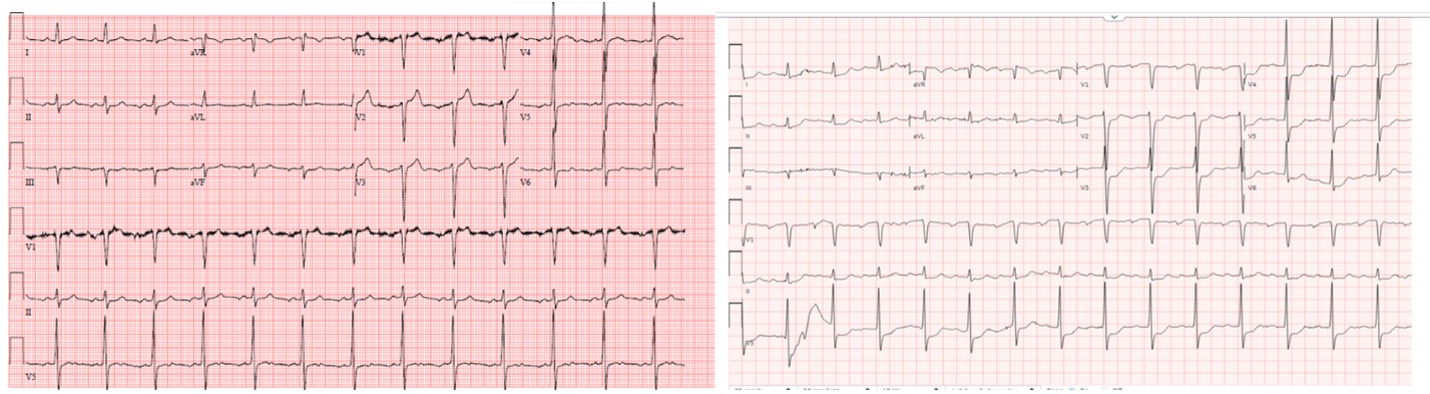
Case Presentation: A 61-year-old male with past medical history of HIV on HAART with undetectable viral load and bicuspid aortic valve (BAV) presented to the hospital with fevers, abdominal pain and diarrhea for three days found to have sepsis with leukocytosis of 13.7×10^3/uL and fever of 39°C, elevated trop of 168ng/L without acute ischemic changes on initial EKG (Fig. 1 Left) and elevated lipase at 229 U/L. Transthoracic Echocardiogram (TTE) showed mildly dilated aortic root to 4.8cm, similar compared to measurement from a CT coronary done in 2020. Patient was otherwise hemodynamically stable and had no cardiac symptoms. Serial troponins down trended and were attributed to type II NSTEMI in the setting of sepsis. Infectious workup was collected including blood cultures. CTAP revealed peri-pancreatic edema around pancreas tail. He was given IV fluids and monitored for presumed acute pancreatitis vs. gastroenteritis off of antibiotics. In the subsequent days, patient had persistent fevers but otherwise felt well with resolution of abdominal pain and diarrhea. On day 3, blood cultures grew Haemophilus parainfluenza and patient was started on Zosyn. On evening of hospital day 4, patient developed acute chest pain and shortness of breath. Repeat EKG (Fig. 1 Right) showed new first-degree AV block and ST depressions in anterolateral leads. Repeat troponin was elevated to 1797ng/L. A STEMI alert was activated and repeat TTE showed aortic root abscess that has likely ruptured into the LVOT and new severe aortic regurgitation. CCU and cardiothoracic surgery were emergently consulted; surgery was planned but patient rapidly decompensated and went into cardiopulmonary arrest. ACLS was unsuccessful and patient expired.
Discussion: Studies show that patients with BAV have significantly increased risk for infective endocarditis (IE), estimated as high as 17-fold compared to the general population. Even though only 1-2% of the general population has a BAV, they account for 25% of IE cases. Studies also show that the age of diagnosis tends to be younger in the BAV population and majority required surgical intervention, though had good long-term survival post surgical intervention. Aortic root dilation is common in those with BAV, which can confound abnormal TTE findings. HACEK (Haemophilus, Aggregatibacter, Cardiobacterium, Eikenella, and Kingella) organisms are a group of gram-negative organisms that account for about 1-3% of endocarditis. They are usually indolent in nature and are slowing growing in culture, which can further delay timely diagnosis that is essential to management, particularly in high risk patient populations such as those with BAV.
Conclusions: BAV is the most common congenital cardiac malformation and pose significantly increased risk for IE, but the risk is often underappreciated. Early diagnosis is crucial to getting timely surgical intervention and improve mortality. For those with history of BAV, it’s important to consider IE in the early differential of sepsis workup even when they do not present with obvious cardiac symptoms.