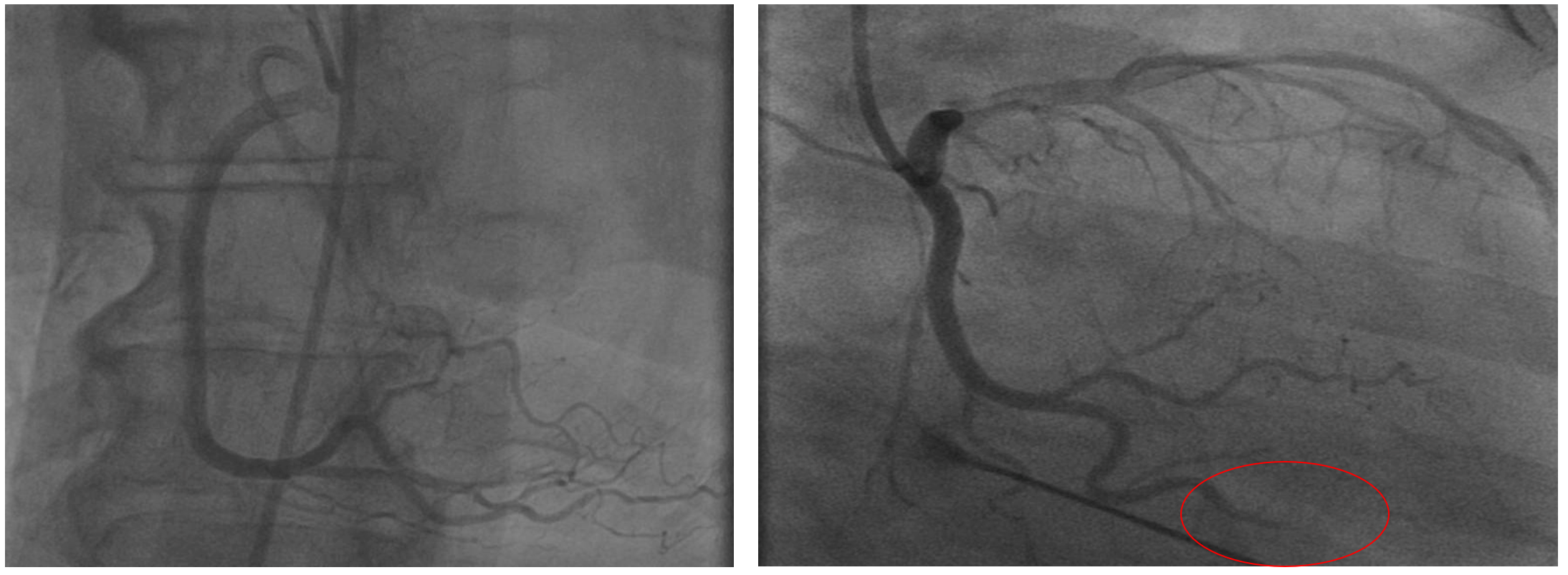
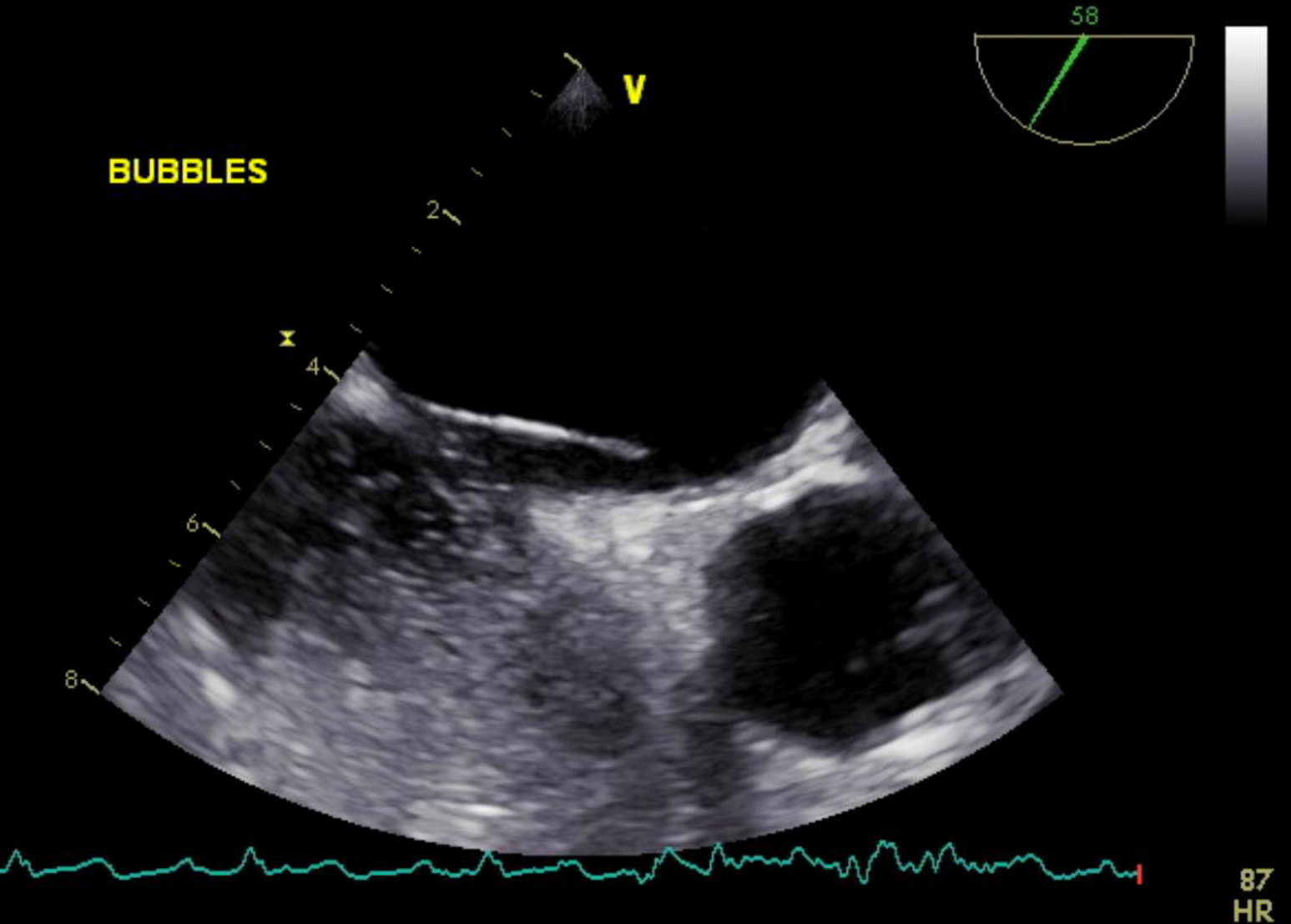
Case Presentation: Our patient is a 69 years old Caucasian female with history of hyperlipidemia, hypertension, diabetes type 2 complicated with ESRD on hemodialysis, and hypothyroidism. Patient presented with symptoms of unstable angina. Lexiscan was abnormal and patient underwent cardiac catheterization which was unremarkable. Pain gradually resolved, and patient was discharged home. One week later patient presented with moderate tightening substernal pain with radiation to neck (classic typical chest pain). ECG showed sinus rhythm with ST elevation in inferior leads. Troponin was elevated. Patient underwent cardiac catheterization which demonstrated moderate inferior wall hypokinesis and complete distal occlusion of circumflex artery. The impression was occlusion is secondary to embolic stenosis. Multiple attempt for aspiration of clot was unsuccessful. TEE with bubble study was consistent with a patent foramen ovale (PFO). Lower extremities duplex was unremarkable. Patient was diagnosed with paradoxical embolization through PFO to coronary arteries.
Discussion: About 6% of patients with Acute myocardial infarction have normal coronary angiography. Differential diagnosis include hypercoagulable state, coronary endothelial dysfunction, inflammation, coronary thrombosis, aortic wall stiffening, cocaine abuse, and paradoxical embolism (PDE). The first case of paradoxical embolism was reported by Cohnheim et al in 1877. PDE presumed when there is evidence of arterial embolization in the absence of a source in the left heart along with an abnormal communication between venous and arterial circulation. Paradoxical coronary embolism to coronary arteries is very rare and is seen in about 5-10% of all PDE phenomena. Transthoracic echo usually shows septal wall-motion abnormalities. Intravenous injection of agitated saline echo-contrast usually reveals PFO. Standard of management for these patients is manual aspiration thrombectomy. Aspiration of intracoronary emboli would avoid clot fragmentation and further distal embolization, and balloon injury associated with angioplasty. Strategies for prevention of future paradoxical embolic event include lifelong oral anticoagulation and/or surgical or transcutaneous closure of PFOs.
Our patient was diagnosed with paradoxical circumflex coronary artery embolism. Although lower extremities duplex was negative for deep vein thrombosis, it is not 100% sensitive test and we should consider other sources of embolism like pelvic venous system. Our patient was treated with long term anticoagulation along with percutaneous closure of the interatrial shunt to prevent the recurrence of another embolic event.
Conclusions: Paradoxical coronary embolism is very rare. Recognition of this condition is very important because these patients are at risk of future fatal embolic phenomena. Transesophageal echocardiogram with bubble study can reveal PFO. Management is cardiac catheterization and aspiration thrombectomy along with anticoagulation and closure of PFOs.