Background: The high volume of handoffs between the Emergency Department (ED) team and the inpatient team on a daily basis makes this a ripe area for care improvement. Effective, safe and organized transitions facilitate high quality and efficient care, while a dysfunctional process negatively affects patients and practitioners and compounds overall hospital congestion and delays in care. In our large urban academic medical center with significant capacity challenges, improving the handoff process without sacrificing safety has been a key goal. Historical efforts to overhaul this workflow have been difficult due to process complexity and the need for a coordinated change across multiple different stakeholder groups.
Purpose: In February 2017, we formed a multi-departmental quality improvement team that included leadership from Medicine, Emergency Medicine, Nursing, Admitting, and Patient Transport. Four workgroups with diverse members were formed focused on (1) communication of expected discharges to Admitting, (2) nursing handoffs, (3) provider handoffs, (4) transport process. Each group developed proposals and performed small pilots. Regular “check-ins” amongst the leads ensured that planned changes were complementary across the global process.
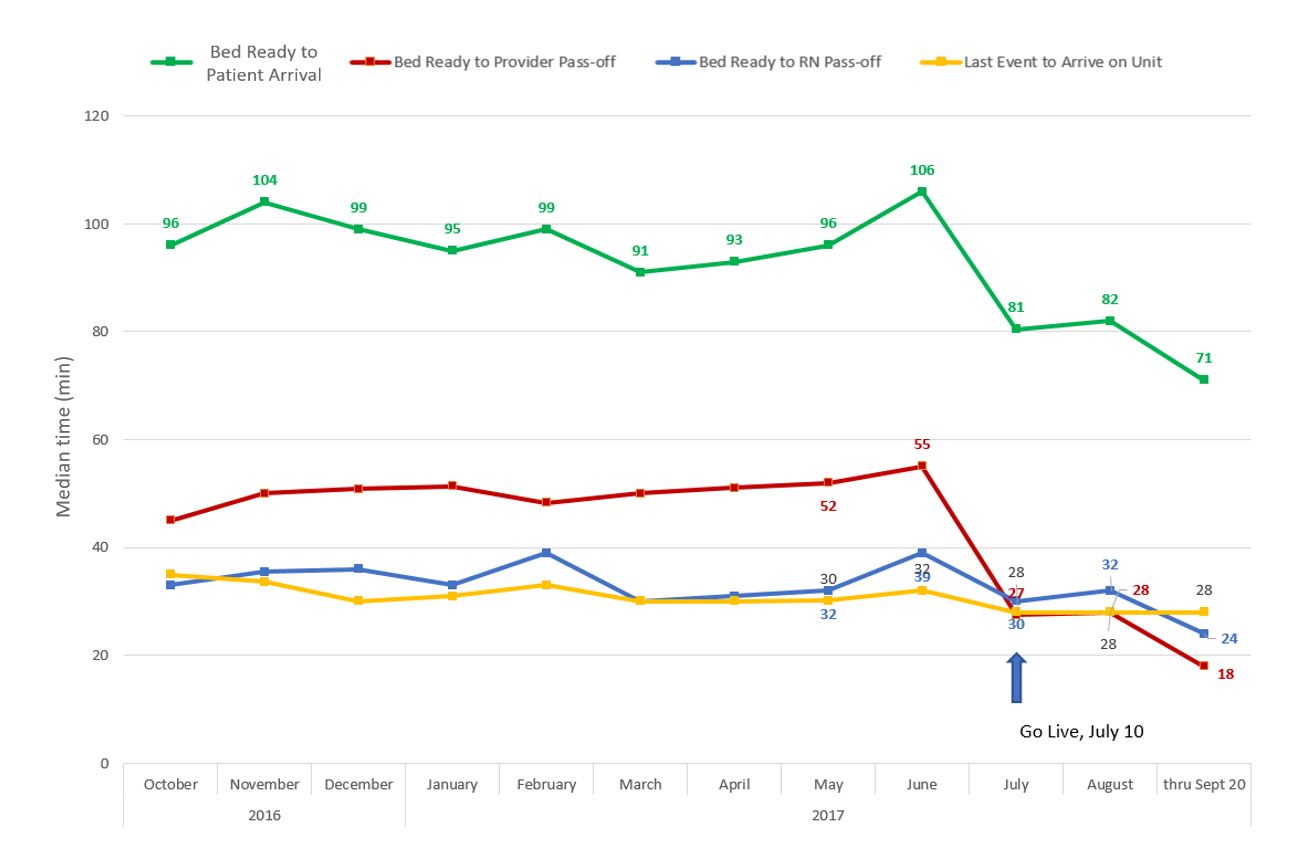
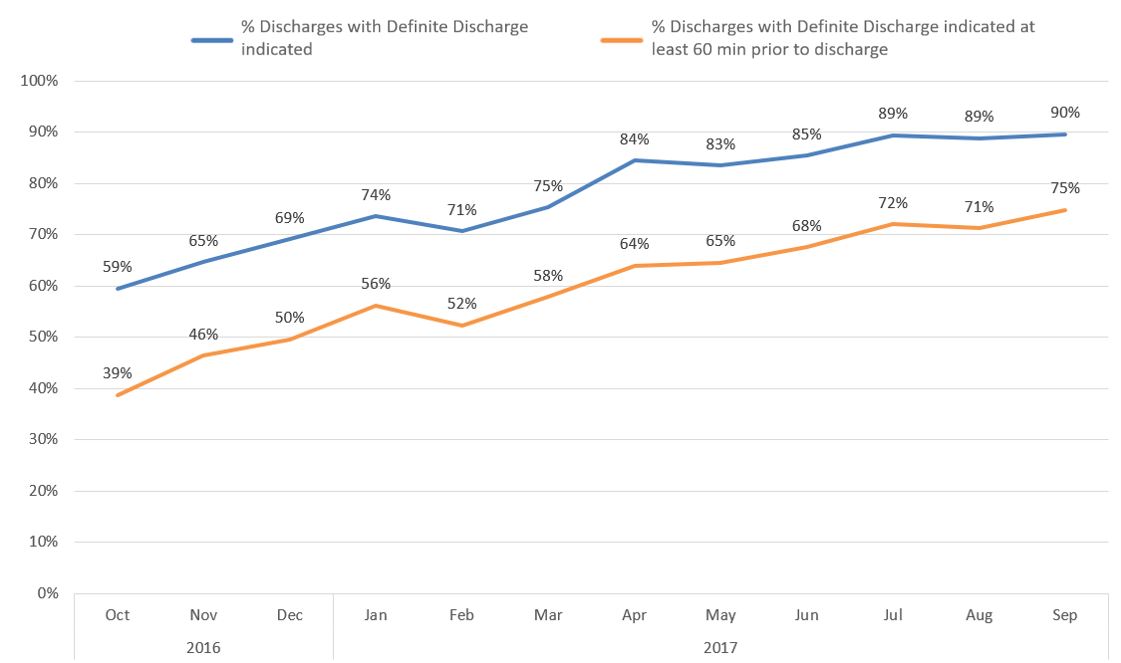
Description: The new handoff process designed with input from all workgroups went live on July 10, 2017. First, expected discharges were more consistently communicated to Admitting, allowing for earlier assignment of new patients to discharge beds. Nursing and provider passoffs could now occur while the discharge bed was being cleaned so a patient was “ready for transfer” when they had a “ready bed”. Nurses and providers created standard passoff templates to aid in efficient and complete verbal handoffs. A new auto-paging tool prompted providers to initiate passoff at the time of bed assignment. Finally, transporter workflows were standardized to increase consistency. With the new process, average time between “ready bed” and patient arrival on the unit improved from 106 to 71 min(Figure 1). Given the volume of ED patients admitted to medicine (daily average 25 patients), this represented a savings of 14.6 patient hours every day. It was felt that these gains were driven by improvements associated with each workgroup: more discharges being communicated to Admitting before discharge (59% to 90%, Figure 2); faster nursing and provider handoffs (32% and 65% reduction in handoff times, respectively); and more consistent transport processes.
Conclusions: By focusing this quality improvement project on multi-disciplinary teams and integrated interventions, we dramatically enhanced a major care transition. Other keys to success were strong leadership engagement, shared accountability around interdependent metrics among the workgroups, and the use of iterative data to drive change.