Background: Sepsis is a major cause of hospital mortality. Moreover, patients who survive sepsis have increased risk for morbidity, rehospitalization, and death in the months after sepsis. To address this, the 2021 Surviving Sepsis Campaign now provides recommendations addressing recovery and longer-term outcomes. We were interested in whether Michigan hospitals are consistently incorporating key elements of sepsis care into their standard practice, and whether self-assessed competency in these practices has improved with time.
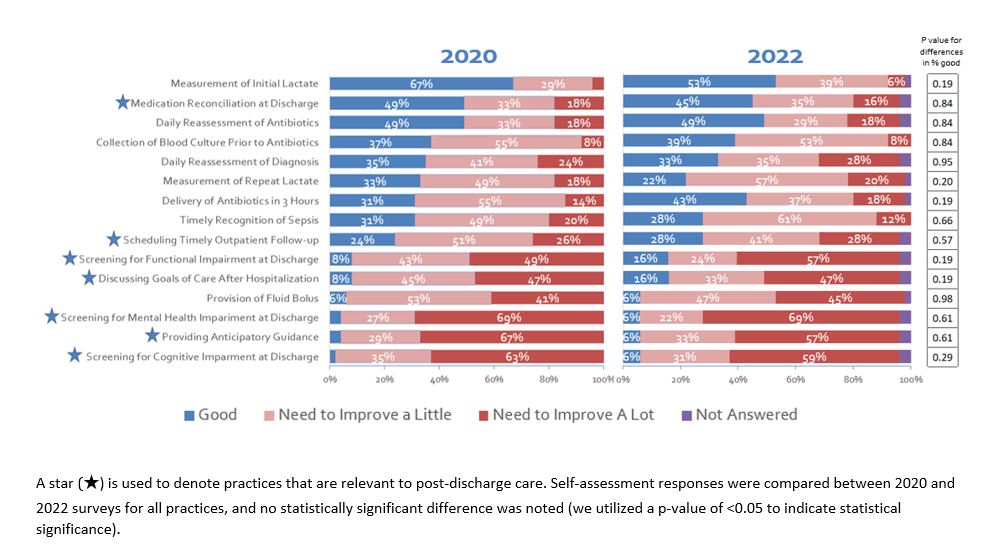
Methods: In December 2020, we surveyed 51 hospitals participating in the Michigan Hospital Medicine Safety Consortium (HMS), a Collaborative Quality Initiative sponsored by Blue Cross Blue Shield of Michigan, on their sepsis initiatives. Hospitals were re-surveyed in April 2022. Surveys were administered via Qualtrics to each hospital’s designated HMS representative who compiled answers from providers at their institution. Surveys included open- and closed-ended questions regarding processes for sepsis quality initiatives, sepsis recognition and treatment, antibiotic stewardship, and hospital discharge management. Hospitals were also asked to assess their performance on various practices, using the following response options: “we need to improve a lot,” “we need to improve a little,” and “we are good at this practice.” We tested for differences in 2022 vs 2020 self-assessment responses with z-tests.
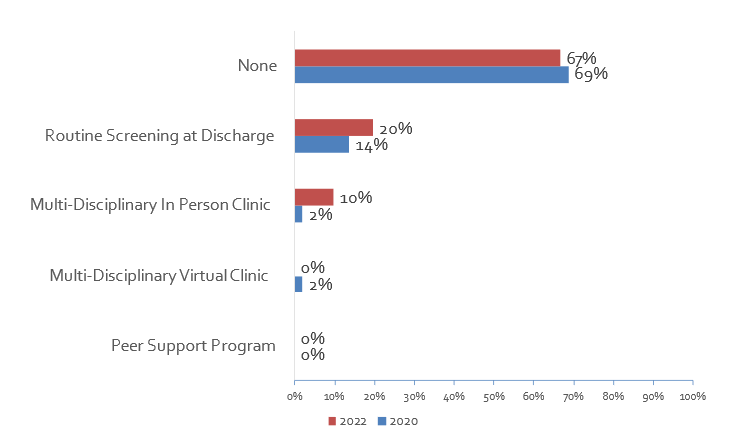
Results: 51 hospitals completed the survey in 2020, a 100% response rate, and the same 51 hospitals responded to the 2022 survey. In 2022, 48 (94.1%) had a sepsis committee and 51 (100%) had a standardized procedure for identifying sepsis. Processes to facilitate rapid sepsis treatment included having hospital protocols/guidelines (n=48; 94.1%), stocking commonly used antibiotics in the ED, ICU, and/or wards (n=45; 88.2%), and having sepsis order sets (n=43; 84.3%). However, formal processes to facilitate sepsis recovery were less common; in 2022, only one-third (n=17; 33.3%) reported having at least one process in place to support recovery (Figure 1). On self-assessment in 2022, measurement of initial lactate was the best practice (n=27; 52.9% “we are good”) followed by daily reassessment of antibiotics (n=25; 49.0% “we are good”). By contrast, self-assessments lagged for recovery-based and discharge-related practices (Figure 2). Practices with the lowest self-assessments included screening for cognitive impairment at discharge (n=3; 5.9% “we are good”), providing anticipatory guidance (n=3; 5.9% “we are good”), and screening for mental health impairment at discharge (n=3; 5.9% “we are good”). Responses to all practices were similar in 2022 vs 2020 (p>0.05 for proportion “we are good” for each practice).
Conclusions: In this serial survey of 51 diverse Michigan hospitals, we show that formal processes to promote recovery from sepsis are rare, and most hospitals identify recovery-based practices as an area for improvement. The lack of a statistically significant change in hospital self-assessed competency in these practices, despite the updated 2021 Surviving Sepsis guidelines, indicates that further interventions are necessary to facilitate improvement. In addition to continuing to improve hospital-based sepsis care, hospitals should consider developing standardized programs for post-discharge sepsis recovery to minimize post-hospitalization morbidity and mortality.