Background: Hospital crowding and subsequent resource strain have been associated with worse patient outcomes and increased length of stay (1–3). As pediatric hospitals face an overwhelming respiratory illness surge in the wake of the COVID pandemic (4–6), improving hospital patient flow is all the more critical. Nonetheless, a substantial proportion of patients, nearly 1 in 4 in one pediatric tertiary care study, who are medically ready experience delays in discharge (7). A growing number of quality improvement initiatives targeting increasing early discharges (EDCs) show promising data on improved emergency department (ED) patient flow without increased readmissions (8–13). At our institution, a 309-bed tertiary care pediatric hospital in south Florida, the pediatric hospital medicine team aimed to increase the percentage of EDCs before noon, from a baseline of 7.6% to an average of 25% over 12 months.
Methods: A multidisciplinary team was created to identify and implement Plan-Do-Study-Act (PDSA) cycles. The first set of interventions included information sharing and team incentives. Information sharing took place in two forms: monthly circulation of an Electronic Medical Record (EMR) dashboard with EDC percentages, and the creation of a shared EMR patient list for daily EDCs. Participation in the QI initiative was included in attending bonus considerations as an incentive, and individual performance was shared at department meetings. The second set of interventions targeted physician and resident workflow: the senior resident and attending communicated early before rounds to assess and accomplish EDCs. Primary outcome was the percentage of early discharges per month, with a secondary outcome of median ED wait time for admission beds. Meanwhile, 7-day ED readmissions percentage was used as a balancing measure.
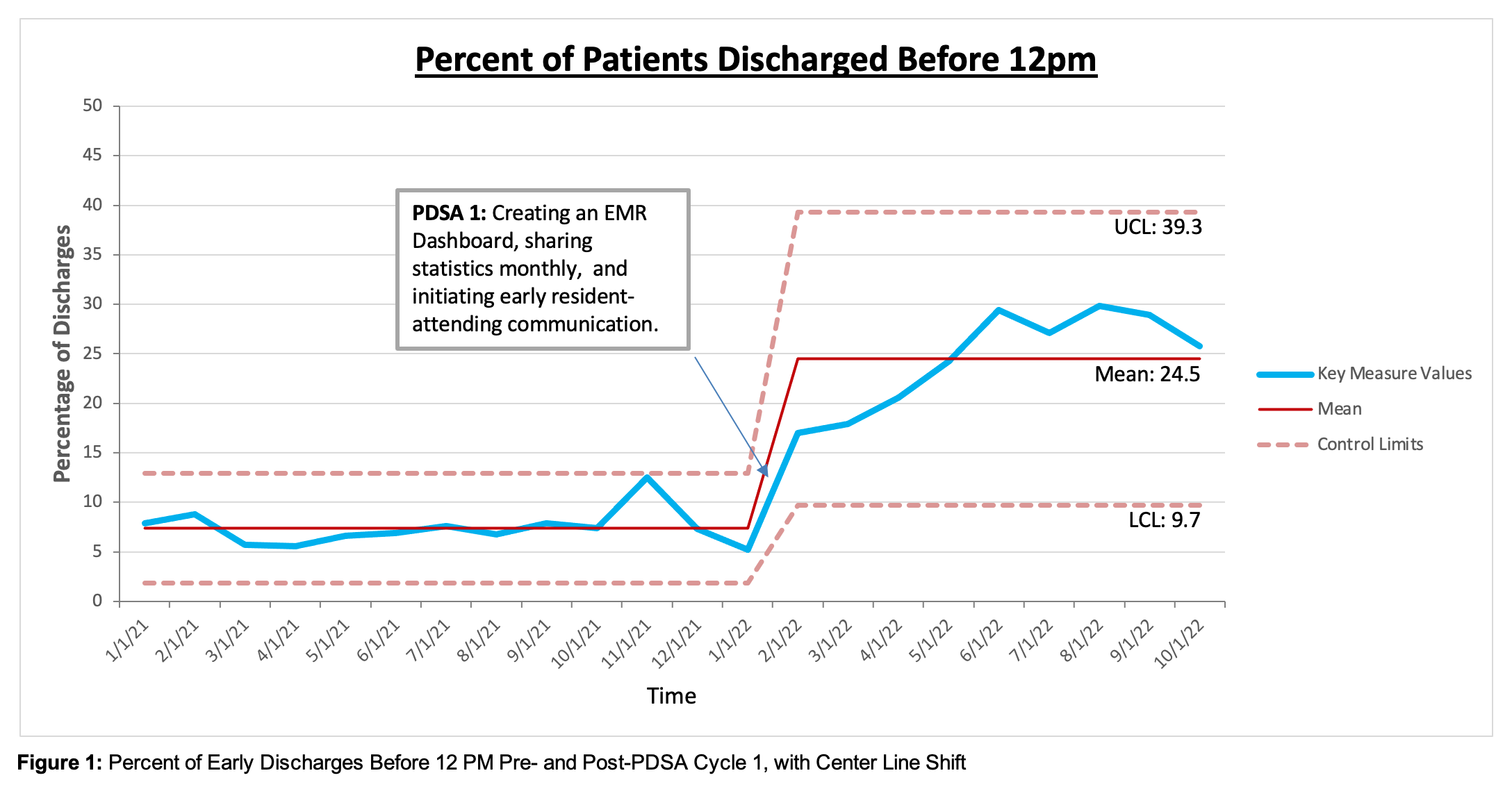
Results: EDCs increased from a baseline 12-month average of 7.6% before project initiation (in January 2022) to a 10-month average of 23% after initiation (P < 0.001). Special cause variation was noted after PDSA cycle 1 with a positive shift in early discharges (see Figure 1). Median ED wait time remained the same at 122 minutes pre- and post-intervention (P = 0.97). Of note, ED admissions have increased from 9223 in the first 10 months of 2021 to 9895 in 2022, which is equivalent to an additional 67 admissions per month. Percentage of 7-day ED readmissions decreased from 2.4% in 2021 to 2% in 2022.
Conclusions: Interventions focused on data sharing, and faculty incentives were associated with a significant increase in pediatric early discharges. These results facilitated timely discharge when patients were medically ready, and avoided unnecessary hospital stay or associated therapies before completion of rounds. These outcomes likely prevented an increase in ED wait time during the current national surge of pediatric admissions.