Background: Multiple organizations have published clinical guidelines on hyperglycemia management in the acute care setting in non-critically ill patients [1–3], and the Society of Hospital Medicine offers additional support through its Glycemic Control program [4]. However, there remains little consensus regarding specific dosing regimens when designing insulin protocols in the inpatient setting. At our institution, a 500-bed hospital within an academic medical center, we implemented a new order set utilizing prandial carbohydrate-counting and correctional insulin scales based on insulin sensitivity factor along with education and usage tracking with provider comparison. We assessed the impact on our primary outcome measure of hypoglycemia and numerous secondary measures.
Methods: We conducted a prospective cohort study. We included encounters for patients on the General Internal Medicine service and point-of-care blood glucose (POC BG) values based on published recommendations [5]. We excluded encounters for patients without diabetes, diagnosed with DKA or HHS, that were pregnant, using an insulin pump, managed by diabetes consultants, and/or receiving no insulin inpatient. An interdisciplinary team developed our new order set and educated providers and pharmacists at time of launch. For 3 months, we tracked provider usage of the new order set and shared results publicly. To assess impact, we compared data across 180-day periods preceding and following the intervention and a 60-day washout period (Mar 2021 to Sep 2021 vs Nov 2021 to May 2022). We measured the number of encounters with hypoglycemia (BG < 70 mg/dL) as well as total daily dose of insulin (units/kg/day), mean glucose, coefficient of variation, percent of BG values within goal range (70-180 mg/dL), number of encounters with hyperglycemia to BG > 300 mg/dL and hypoglycemia to BG < 60 mg/dL, length of stay, 30-day readmission, and hospital mortality. We compared baseline characteristics and unadjusted outcome measures using Welch’s t test or Wilcoxon rank sum test as appropriate. We compared adjusted outcomes using generalized linear models with a log link function and gamma distribution for continuous outcomes and multivariable logistic regression for categorical outcomes.
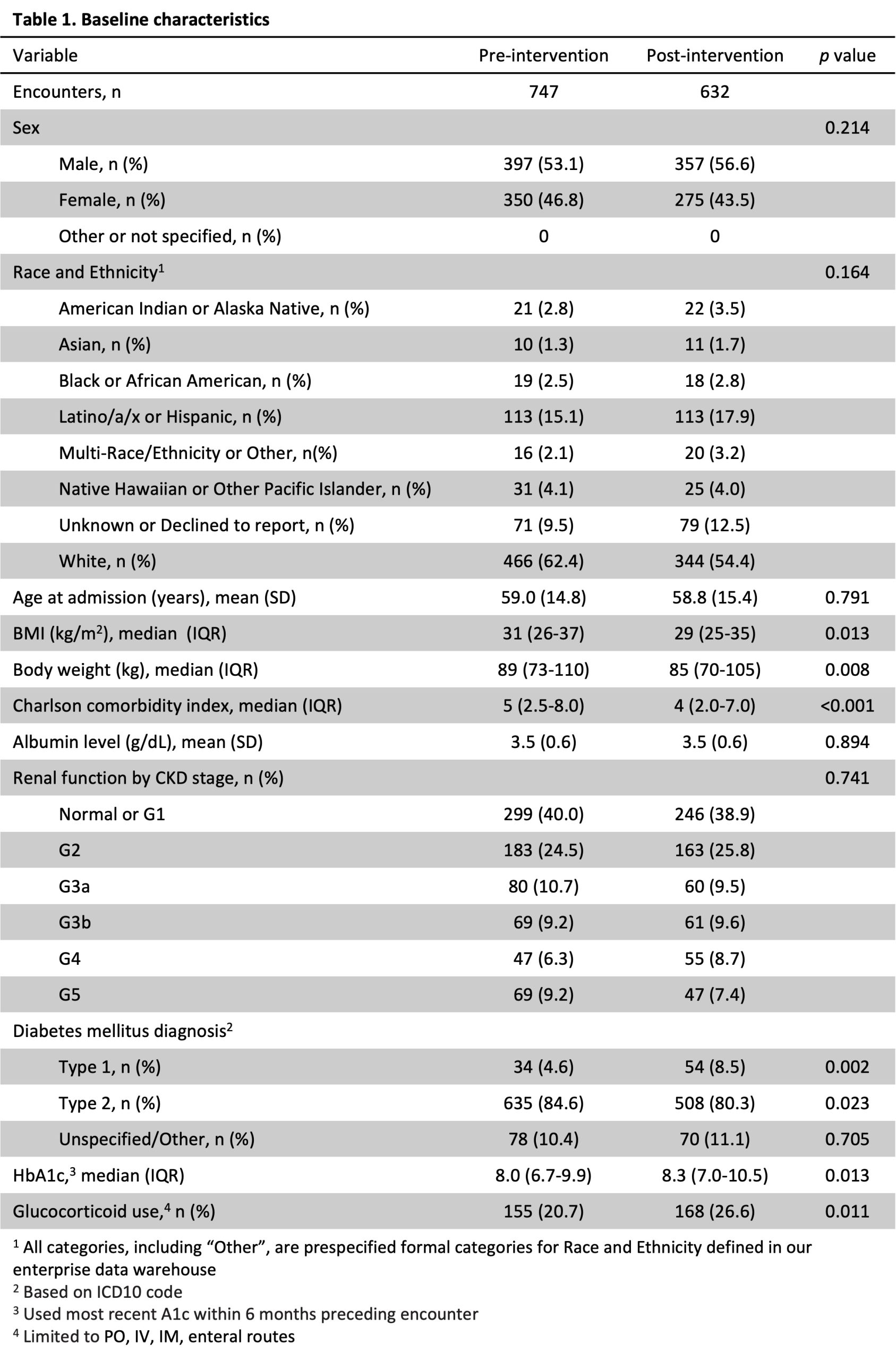
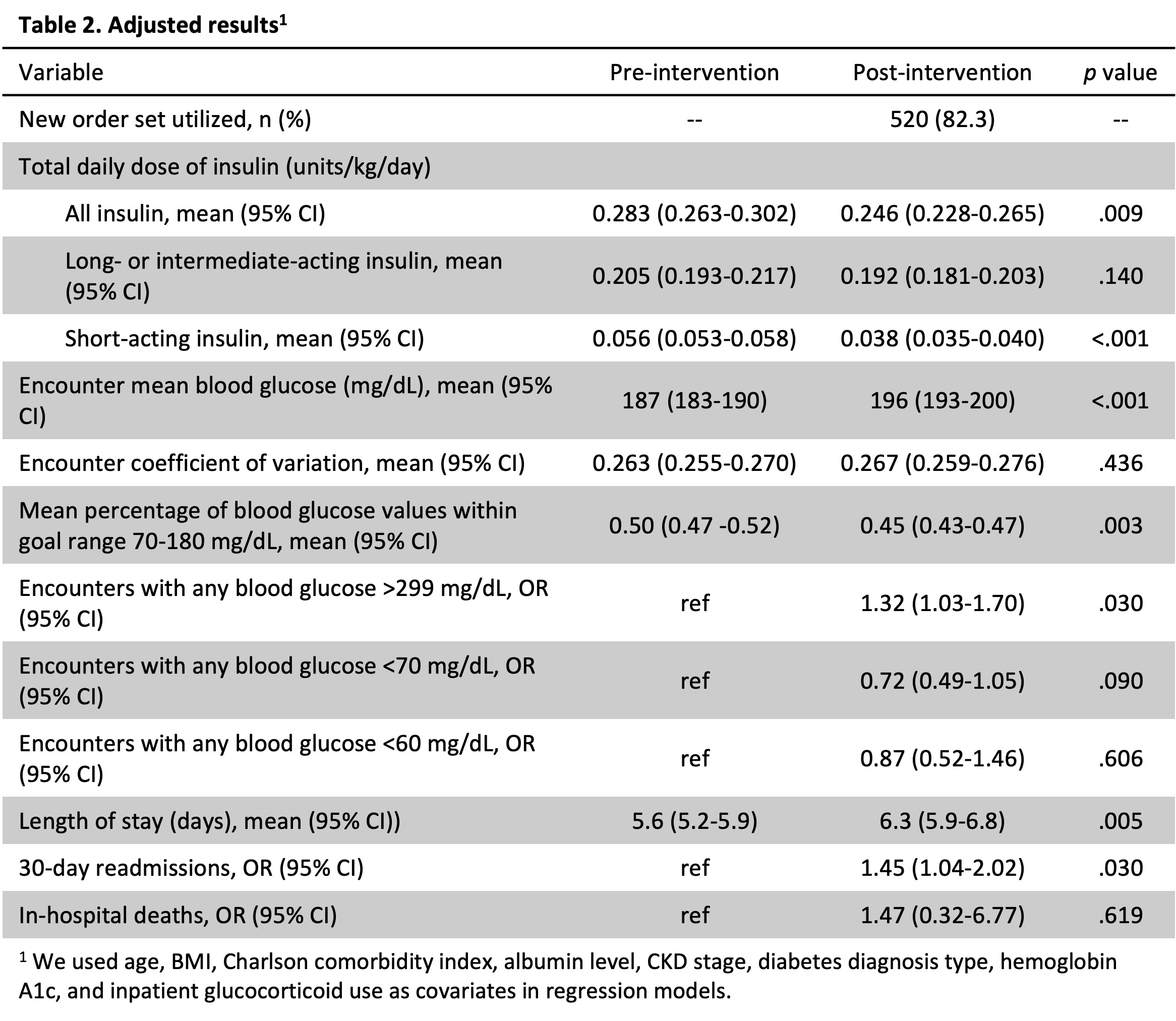
Results: Of 7883 hospital discharges from the General Internal Medicine service, we included 1379 in our final data based on exclusion criteria. Baseline characteristics are summarized in Table 1. 1520 (82.3%) of encounters post-intervention utilized the new order set. The intervention was associated with a significant reduction in insulin use (0.037 units/kg/day, p = .009) and non-significant reduction in risk of hypoglycemia < 70 mg/dL (OR = 0.72, 95% CI [0.49-1.05]). It was associated with a higher mean BG (187 vs 196 mg/dL, p < .001) and risk of hyperglycemia >300 mg/dL (OR = 1.32, 95% CI [1.03-1.70]), as well as a lower percentage of BG within target range (50 vs 45%, p = .003). We did note a significant increase in length of stay (5.6 vs 6.3 days, p = .005) and risk of 30-day readmission (OR = 1.45, 95% CI [1.04-2.02]).
Conclusions: We demonstrated good uptake of the new order set. Our intervention was associated with a reduction in insulin usage and nonsignificant trend to reduced risk of hypoglycemia, though it was associated with increased risk of hyperglycemia. We did note an associated increase in length of stay and risk of 30-day readmission, though this may be the result of a few extreme outliers and the Delta and Omicron waves of the COVID-19 pandemic.