Background: According to the CDC, at least 300,000 people older than 65 are hospitalized for hip fractures annually. Society of Hospital Medicine recognizes geriatric care as one of the core competencies, and hospitalists frequently provide care to geriatric hip fracture patients. Clearly hospitalists need to be competent providing care to such patients. Our goal was to design an effective online module for the hospitalist faculty and geriatric fellows that covered basic principles of care in geriatric hip fracture patients at an academic medical center.
Methods: With the expertise of a geriatrician, we designed an interactive case-based online educational module, delivered through a virtual patient software available at our institution. The case started with a patient presenting with a hip fracture and went through various common medical problems during hospitalization before post-operative discharge. We focused on recent evidence about mortality associated with hip fractures, guidelines about pain control, guidelines about deep venous thrombosis prophylaxis, guidelines about delirium management, recent evidence about nutrition, KATZ ADL scale and Clinical Frailty Scale.
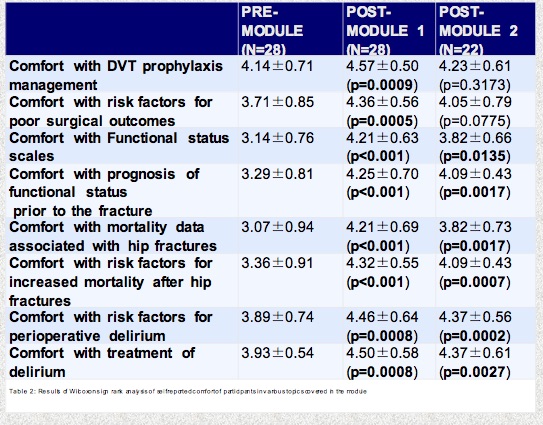
Evaluation of the curriculum consisted of pre and post-test surveys delivered through REDCAP software immediately after the module and at 30-60-day point. The surveys assessed comfort and knowledge levels based on questions designed by the authors. We used the Wilcoxon Sign rank test to analyze significant increase in comfort level and knowledge scores. Participants were asked to rank the helpfulness of the module based on a 5-point Likert scale.
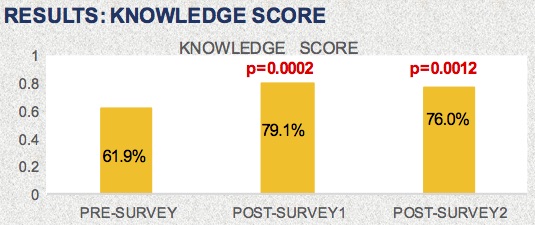
Results: The curriculum was delivered to 52 participants and we had a response rate of 63.5% (N = 33) in the immediate post- module survey. In end we had 28 matched Post-module survey 1 and 22 matched Post-module Survey 2. We noted a significant and sustained increase in self-reported comfort level of participants with regard to using functional scales for prognosis, evidence about mortality related to hip fractures, factors that increase risk of delirium, delirium treatment in both surveys. In the Post-module survey-1 there was a significant increase in self-reported comfort level with regards to deep venous thrombosis prophylaxis and risk factors for surgical outcomes, but this was not sustained in the second survey. Importantly, there was a significant and sustained increase in knowledge base noted (p=0.002 and p=0.0012). Majority of the participants reported module was helpful or very helpful in both surveys.
Conclusions: Our module led to an increase in comfort and knowledge of participants, with evidence of knowledge retention in our 30-60-day survey. Thus, this convenient, electronic module design was an effective and educational tool for the hospitalist faculty, and may be used for many educational topics for busy clinicians. Further evaluation of the curriculum will measure sustained knowledge base and changes in provider behavior.