Background: Despite years of intense focus, inpatient and observation readmission rates remain high and largely unchanged. Little robust evidence exists to guide hospitals in the selection of interventions effective at reducing 30 day readmissions in real-world settings. Our local healthcare system incorporated the most recent recommendations for preventing readmissions into a comprehensive program called Transition Services (TS). This program bridges inpatient, outpatient, and home settings, providing patients virtual and in person access to a dedicated multidisciplinary team for 30 days We aimed to evaluate the hypothesis that referral to the TS program results in lower 30 day readmission rates compared to usual care in a population discharged to home and at high-risk for readmission.
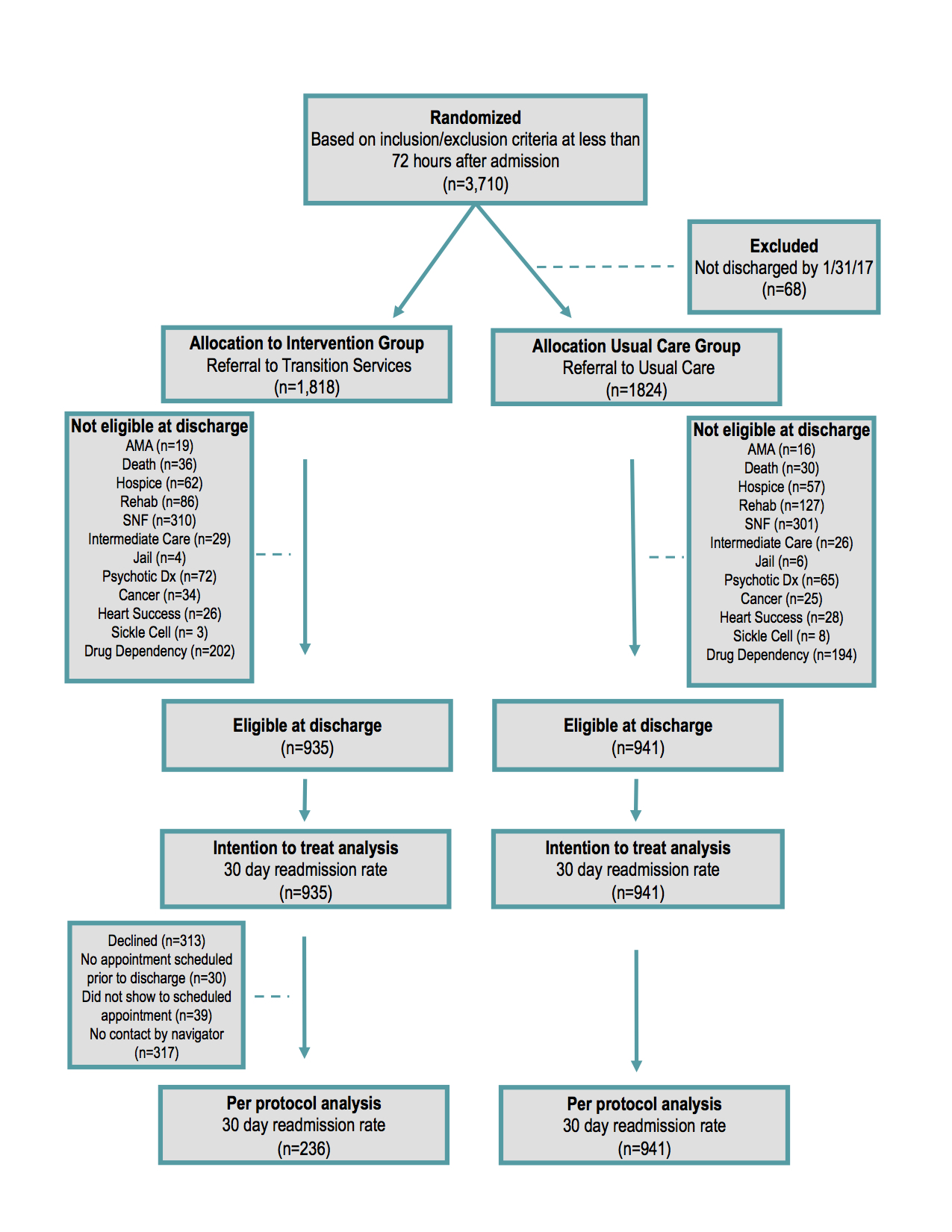
Methods: Aiming to Improve Readmissions Through InteGrated Hospital Transitions (AIRTIGHT) is a non-blinded, pragmatic randomized controlled trial with patients allocated to receive either a referral for the hospital transition program or usual care. AIRTIGHT was conducted within 2 hospitals in Charlotte, NC from February 2016 to January 2017. Patients were eligible if during the first 72 hours of admission they were: over the age of 18, seen by a hospitalist, and identified as high-risk for readmission using a risk scoring model. The primary outcome was the 30 day, unplanned, inpatient or observation readmission rate to any of the system’s 40 hospitals. The primary analysis followed the intention-to-treat principle for all patients discharged to home (Figure 1).
Results: 1,876 patients were allocated to a TS program referral (n=935) or usual care (n=941) and discharged to home. The 30 day readmission rate was 15.2% in the TS group and 16.3% in the usual care group (RR 0.93; 95% [CI, 0.76 to 1.15]; P = 0.52). TS patients with a diagnosis of sepsis had lower 30 day readmission rates (RR 0.49; 95% [CI, 0.24 to 0.97]; P = 0.03); but rates were not different for those with congestive heart failure or pneumonia. Patients referred to TS and readmitted, had less Intensive Care Unit admissions 15.5% vs. 26.8% (RR 0.74; 95% [CI, 0.59 to 0.93]; P = 0.02).
Conclusions: For healthcare systems seeking to avoid 30 day readmission penalties, the evidence remains mixed. In this trial, when analyzed within a real-world population health framework, referral of high-risk patients to a transitions program did not lead to reductions in 30 day readmissions. However, the results do suggest improvements in certain patient outcomes, particularly in secondary analyses for those patients who chose to participate. This intervention, like the majority of population health interventions undergoing pragmatic evaluation, suffers from a high crossover rate into usual care (74.8%), highlighting the need for innovative approaches to address the difficult challenge of engaging high-risk populations within a very complex healthcare environment.